When Cancer Resurfaces: Late Metastasis After Partial Laryngectomy
S Moujrid*, R Marouf, M Loudghiri, W Bijou, Y Oukessou, S. Rouadi, R Abada, M Roubal and M Mahtar
Department of Otolaryngology, Head and Neck Surgery, Ibn Rochd University Hospital, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
*Corresponding Author: Sara Moujrid, Department of Otolaryngology, Head and Neck Surgery, Ibn Rochd University Hospital, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Citation: Moujrid S, Marouf R, Loudhghiri M, Bijou W, Oukessou Y, et al. When Cancer Resurfaces: Late Metastasis After Partial Laryngectomy. J Can Ther Res. 4(1):1-10.
Received: December 01, 2024 | Published: December 12, 2024
Copyright© 2024 Genesis Pub by Moujrid S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/JCTR.2024.4(1)-38
Abstract
Laryngeal cancer poses significant challenges in treatment due to its propensity for recurrence, particularly following initial interventions such as partial laryngectomy. Despite advancements in surgical techniques and adjuvant therapies, including postoperative radiotherapy, the risk of local recurrence remains a critical concern.
We report the case of a 59 years old male patient, operated for supracricoid partial laryngectomy with bilateral lymph node dissection, on an ulcerative and infiltrative carcinoma of the glottic region, who developed recurrence two years post-surgery. The cervical CT scan revealed thickening of the left lateral wall of the larynx at the glottic level with a low cervical subcutaneous mass. The biopsy revealed an invasive squamous cell carcinoma. The patient underwent a total laryngectomy surgery.
Positive surgical margins are associated with higher recurrence rates, emphasizing the need for intraoperative margin biopsies. Clinical follow-up for at least three years is essential, as nearly 90% of recurrences occur within this period.
Keywords
Laryngeal cancer; Surgical technique; Supracricoid partial; Partial laryngectomy; Radiotherapy; Anterior cervical mass.
Introduction
Laryngeal cancer, particularly glottic and supraglottic variants, remains a significant clinical challenge due to its potential for recurrence following treatment. Partial laryngectomy, often accompanied by bilateral lymph node dissection and postoperative radiotherapy, is a common intervention aimed at achieving local control of the disease. However, despite these comprehensive treatment approaches, the risk of recurrence persists.
This article presents a case study of a patient who underwent partial laryngectomy with intact surgical margins and thorough lymphatic assessment, followed by adjuvant radiotherapy. Notably, this patient experienced a recurrence of cancer two years post-surgery, highlighting the complexities involved in managing laryngeal malignancies.
Previous studies indicate that recurrence rates for laryngeal cancer can vary significantly, with local recurrences occurring predominantly within the first three years after treatment. Factors such as tumor stage, nodal involvement, and the specific anatomical subsite contribute to the likelihood of recurrence. In our case, the development of recurrent disease despite initial negative margins and comprehensive treatment underscores the unpredictable nature of laryngeal cancer progression.
This article aims to explore the implications of our findings within the broader context of laryngeal cancer management, examining risk factors associated with recurrence and discussing strategies for surveillance and intervention in similar cases. By analyzing this case alongside existing literature, we seek to enhance understanding and improve outcomes for patients at risk of recurrent laryngeal cancer.
Case Report
We report the case of a 59 years old male patient, operated for supracricoid partial laryngectomy in 2022 with bilateral lymph node dissection, followed by Radiotherapy; on an ulcerative and infiltrative carcinoma of the glottic region, affecting the anterior commissure. No signs of metastasis lymph nodes on pathological examination. The patient consulted our ENT department for an anterior cervical mass (Figure 1).
Figure 1: Image showing the anterior cervical mass.
The history of the disease dates to 2 years after the surgery, with the appearance of a mobile, firm and painless anterior cervical mass, progressively increasing in size, complicated by an inspiratory dyspnea that required an emergency tracheotomy.
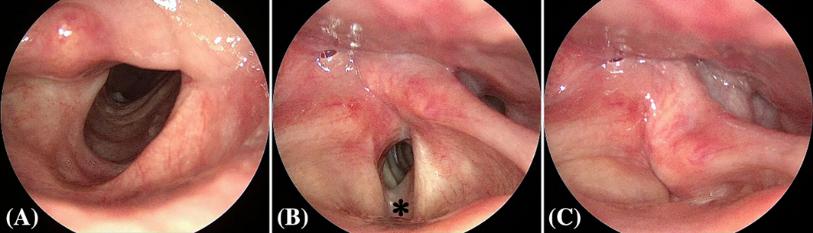
On physical examination, the patient was in good general condition, tracheotomized. On cervical inspection, a mass is noted in the anterior cervical region, located at the site of the tracheostomy opening, measuring approximately 2 cm, fixed, immobile on swallowing, with no palpable lymph nodes. On nasofibroscopy, the glottic space is free.
On the suspension laryngoscopy, the base of the tongue, piriform sinus and the proximal part of the esophagus were intact. The rest of the physical examination was normal.
As part of the paraclinical examination, a cervical CT scan revealed thickening of the left lateral wall of the larynx at the glottic level, with a nonspecific appearance, and a low cervical subcutaneous mass with a suspicious appearance. The mass also comes into contact with the left lobe of thyroid gland. (Figure 2).
Figure 2: CT scan image showing the location of the process which comes into contact with the antero-lateral part of the larynx (orange arrow) and with the left lobe of thyroid gland (black arrow).
A cervical MRI revealed a suprasternal tissue formation in the anterior cervical wall, with T1 hyposignal and T2 heterogeneous hypersignal, enhanced early on injection of Gadolinium (Figure 3).
Figure 3: MRI image showing the location of the process which comes into contact with the lateral wall of the larynx (white arrow) and the anterior sus sternal part (orange arrow).
A biopsy of the mass was performed, revealing a pathological result consistent with a invasive squamous cell carcinoma. On the basis of these data, the decision in a multidisciplinary consultative meeting was to perform a laryngectomy totalization with surgical resection of the mass.
On definitive pathological examination, all the margins of the specimen were intact, and the appearance were effectively consistent with a reccurence of a squamous cell carcinoma. The physical examination on the follow-up consultations was normal.
Discussion
Laryngeal cancer is the second most common cancer in the head and neck region, after skin cancer. In Morocco, laryngeal cancer ranks 16th, accounting for 2% of all diagnosed cancers and responsible for 770 cancer-related deaths annually, representing 2.2% of all cases It is consequently seen as a major public health concern [1-2].
The management of laryngeal cancers has currently seen considerable progress in terms of exploration and treatment, with the ultimate goal of preserving physiological functions as much as possible.
The latest approach in the treatment of laryngeal tumors focuses not only on ensuring oncological safety but also on enhancing the patient's quality of life by promoting natural breathing and swallowing, while striving to maintain an acceptable voice quality to preserve social interactions [3-7].
In the field of surgery, efforts have been made to develop techniques that preserve part of the laryngeal structure, ensuring the retention of the laryngeal sphincter and respiratory function while achieving oncological outcomes comparable to total laryngectomy (TL). Currently, for the treatment of glottic and supraglottic tumors in intermediate to advanced stages, supracricoid partial laryngectomy (SCPL) is the surgical procedure that has received unanimous approval for its oncological and functional results [8-11].
Functional outcomes of TL surgery are generally considered superior to those of open surgery, and in many cases, they are comparable to those achieved with radiotherapy and robotic surgery. Other advantages of TL surgery include lower morbidity and mortality rates, a reduced need for tracheotomy, and shorter hospital stays [12-14].
While TL surgery was once thought to be suitable only for early-stage (T1, T2) glottic and supraglottic cancers, research by Ambrosch et al. and Mannelli et al. has demonstrated its effectiveness in treating advanced-stage (T3, T4) cancers as well [15-16].
One of the key oncological challenges during partial laryngectomy is the presence of tumors at the surgical margins. Positive surgical margins are associated with higher rates of recurrence, reduced local control, lower disease-specific survival, and decreased overall survival. As a result, it is recommended to perform biopsies of the surgical margins for intraoperative frozen section analysis. Fang et al. reported that positive surgical margins were often linked to early local recurrence and poor prognosis in early-stage glottic cancers. Similarly, Nakayama et al. demonstrated that positive surgical margins in open surgery were associated with early recurrence and higher mortality rates in 61 cases of supracricoid laryngectomy [17-18].
The safety margins should ideally be 1 to 2 mm around the tumor to ensure complete excision, which is essential to prevent recurrence [19-20].
In our case, the patient underwent a partial laryngectomy with clear margins (5mm from the inferior and anterior margin, 8mm from the left lateral margin, 10mm from the right lateral margin, and 15mm from the base of the tongue), which makes local recurrence very unusual.
N classification was also been related to a higher risk of recurrence. In a study conducted by Crosetti et al. on 819 patients affected by laryngeal cancer, neck dissection was performed with either elective or curative intent in 86% of patients. Neck recurrences were detected in 25.5% of pN+ patients and in 4.6% of pN0 patients [21].
Our patient underwent a preventive neck dissection, which included 23 lymph nodes on the right side and 32 lymph nodes on the left side. The pathological examination did not reveal any signs of metastasis.
The treatment landscape for recurrent laryngeal cancer involves a combination of surgical interventions, reirradiation, and careful monitoring of high-risk populations. A study from Memorial Sloan Kettering Cancer Center reviewed 241 patients with recurrent laryngeal cancer, with total laryngectomy being the most common salvage procedure, performed in 74% of cases. The study reported a 2-year disease-specific survival rate of 74% and a 5-year survival rate of 57%, with tumor location and perineural invasion identified as key prognostic factors [22].
In contrast, a retrospective analysis on the efficacy and toxicity of reirradiation in 129 patients with locally recurrent laryngeal cancer found a 2-year overall survival rate of approximately 40.6%. The study suggested that reirradiation could be a feasible option for small local recurrences, though it stressed the importance of careful patient selection to minimize the risk of severe toxicities [23].
Clinical follow-up should be conducted for at least three years, as almost 90% of LSCC recurrences are observed within the first three years following the initiation of treatment [24].
Conclusion
The treatment of laryngeal cancer, should be approached with an aggressive strategy to optimize outcomes and minimize the risk of recurrence. Despite the best possible interventions, including surgery and adjuvant therapies, recurrence remains a possibility that cannot be overlooked. Therefore, diligent follow-up care is essential; we recommend monitoring every six weeks for the first three years post-treatment, ideally by the physician who managed the initial care. This proactive approach is crucial for early detection and timely intervention in the event of recurrence, ultimately enhancing patient prognosis and quality of life.
References
- Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, et al. (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 144(8):1941-1953.
- Chu EA, Kim YJ. (2008) Laryngeal cancer: diagnosis and preoperative work-up. Otolaryngol Clin North Am. 41: 673-95.
- Chevalier D, Piquet JJ. (1994) Subtotal laryngectomy with cricohyoidopexy for supraglottic carcinoma: review of 61 cases. Am J Surg. 168(05):472–473.
- de VincentiisM, Minni A, Gallo A. (1996) Supracricoid laryngectomy with cricohyoidopexy (CHP) in the treatment of laryngeal cancer: a functional and oncologic experience. Laryngoscope. 106(9 Pt 1):1108–14.
- Laccourreye O, Brasnu D, Périé S, Muscatello L, Ménard M, et al. (1998) Supracricoid partial laryngectomies in the elderly: mortality, complications, and functional outcome. Laryngoscope. 108(02):237–42.
- Naudo P, Laccourreye O, Weinstein G, Hans S, Laccourreye H, et al. (1997) Functional outcome and prognosis factors after supracricoid partial laryngectomy with cricohyoidopexy. Ann Otol Rhinol Laryngol 106(04):291–96.
- Brasnu D, Menard M, Fabre A, Janot F, Laccourreye H. (1988) [Partial supracricoid laryngectomies: techniques, indications and results]. J Otolaryngol. 17(04):173–78.
- Gong H, Zhou L, Wu H. (2019) Long-term clinical outcomes of supracricoid partial laryngectomy with cricohyoidoepiglottopexy for glottic carcinoma. Acta Otolaryngol. 139(09):803–09.
- Crosetti E, Bertolin A, Molteni G. (2019) Patterns of recurrence after open partial horizontal laryngectomy types II and III: univariate and logistic regression analysis of risk factors. Acta Otorhinolaryngol Ital. 39(04):235–43.
- Succo G, Fantini M, Rizzotto G. (2017) upratracheal partial laryngectomy: indications, oncologic and functional results. Curr Opin Otolaryngol Head Neck Surg. 25(02):127–32.
- Succo G, Crosetti E, Bertolin A. (2016) Benefits and drawbacks of open partial horizontal laryngectomies, Part A: Early- to intermediate- stage glottic carcinoma. Head Neck. 38(1):333–40.
- Tufano RP, Stafford EM. (2008) Organ preservation surgery for laryngeal cancer. Otolaryngol Clin North Am. 41: 741-55.
- Iro H, Waldfahrer F, Altendorf-Hofmann A, Weidenbecher M, Sauer R, et al. (1998) Transoral laser surgery of supraglottic cancer: follow-up of 141 patients. Arch Otolaryngol Head Neck Surg. 124: 1245-50.
- Agrawal A, Moon J, Davis RK, Sakr AW, Giri SPG, et al. (2007) Transoral carbon dioxide laser supraglottic laryngectomy and irradiation in stage I, II, and III squamous cell carcinoma of the supraglottic larynx: report of Southwest Oncology Group Phase 2 Trial S9709. Arch Otolaryngol Head Neck Surg. 133: 1044-50.
- Ambrosch P, Gonzalez-Donate M, Fazel A, Schmalz C, Hedderich J. (2018) Transoral laser microsurgery for supraglottic cancer. Front Oncol. 8:158.
- Mannelli G, Lazio MS, Luparello P, Gallo O. (2018) Conservative treatment for advanced T3-T4 laryngeal cancer: meta-analysis of key oncological. Eur Arch Otorhinolaryngol. 275:27-38.
- Fang TJ, Courey MS, Liao CT, Yen TC, Li HY. (2013) Frozen margin analysis as a prognosis predictor in early glottic cancer by laser cordectomy. Laryngoscope. 123:1490-5.
- Nakayama M, Okamoto M, Iwabuchi K, Mikami T, Seino Y. (2011) Clinical significance of intraoperative surgical margin study in supracricoid laryngectomy. Auris Nasus Larynx. 38:261-5.
- Remacle M, Lawson G, Hantzakos A, Jamart J. (2009) Endoscopic partial supraglottic laryngectomies: techniques and results. Otolaryngol Head Neck Surg. 2009 Sep;141(3):374-81.
- SFORL. (n.d.). Carcinome épidermoïde du larynx. Société Française d'ORL
- Crosetti E, Bertolin A, Molteni G, Bertotto I, Balmativola D, et al. (2019) Patterns of recurrence after open partial horizontal laryngectomy types II and III: univariate and logistic regression analysis of risk factors. Acta Otorhinolaryngol Ital. 39(4):235-243.
- Mimica X, Hanson M, Patel SG, McGill M, McBride S, et al. (2019) Salvage surgery for recurrent larynx cancer. Head Neck. 2019 Nov;41(11):3906-3915.
- Yamazaki H, Suzuki G, Aibe N. (2023) Reirradiation for local recurrence of oral, pharyngeal, and laryngeal cancers: a multi-institutional study. Sci Rep. 13;3062.
- Brandstorp-Boesen J, Sørum Falk R, Folkvard Evensen J, Boysen M, Brøndbo K. (2016) Risk of Recurrence in Laryngeal Cancer. PLoS One. 11(10):0164068.

