Vacancies Regulation Center: A Legal and Functional Analysis
Tricia Bogossian*
Santa Úrsula University Graduate Program Master In Labor Management For Quality Of The Built Environment
*Corresponding author: Tricia Bogossian, Santa Úrsula University Graduate Program Master In Labor Management For Quality Of The Built Environment
Citation: Bogossian T. (2024) Vacancies Regulation Center: A Legal and Functional Analysis. J Clin Pract Med Case Rep. 1(2):1-16.
Received: July 01, 2024 | Published: July 23, 2024
Copyright© 2024 genesis pub by Bogossian T. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
This dissertation aims to analyze the vacancies regulation center within the scope of Law, seeking to understand its structure, functioning and impact on the distribution of resources in the Single Health System (SUS). The Vacancies Regulation Center is a mechanism used by several countries as a way of organizing the supply and demand for medical services, aiming to guarantee equal and efficient access to available resources. The methodology used consists of this process of analyzing bibliographies in order to conjecture relevant information on the topic. It was concluded that it is the State's responsibility to promote adequate investments in public health, strengthening the SUS as a whole. Only with the joint commitment of managers, health professionals and civil society will it be possible to achieve the SUS's greatest objective: provide quality and accessible healthcare for all Brazilians, building a fairer, more inclusive and healthier society. The SUS Vacancies Regulation Center is one of the fundamental pieces in this journey, and its continuous improvement is essential for the Brazilian public health system to reach its full potential and be a reference for excellence in health care for the population.
Keywords
Regulation Center; Vacancies; SUS.
Introduction
The State, through the Federal Constitution of 1988, made access to quality healthcare a right for all Brazilian individuals. In principle, since it is the State's duty to provide for the population, this contribution encompasses both the precepts of prevention and treatment, guaranteeing complete and free healthcare.
Today, the current health project is called the Single Health System (SUS), being the means established by the states to provide care for the population. However, its historical process went through several modifications and legislative movements until it was included in its current term.
In Brazil, the SUS Vacancies Regulation Center has great importance in the management and allocation of health services. Acting as a fundamental mechanism, its objective is to increase the effectiveness, openness and equity in the accessibility of different levels of medical assistance within the country's public health system.
In this sense, the objective of this study is to analyze the vacancies regulation center within the scope of Law, seeking to understand its structure, functioning and impact on the distribution of resources in the SUS.
The methodology used consists of this process of analyzing bibliographies in order to conjecture relevant information on the topic. The bibliographic review methodology allows the researcher to consolidate several theoretical contributions in order to reinforce the approach he seeks, in the face of similar themes. This stage involves analyzing and extracting pertinent data that enable the achievement of the objectives proposed in the study.
The Public Health System – SUS
In the mid-1920s, government bodies began to consider the public health process as an appropriate responsibility in order to offer a quality of life to the population at affordable or even zero costs.
According to [1], a program stipulated by the federal government was created with the possibility of implementing several health stations in urban regions present in Brazil.
Before this movement towards the establishment and resumption of government in the area of health care, the properties that carried out these functions were established by the private sectors.
Even with the possibility of access to everyone through health care, there were processes of distinction in relation to the service model developed for each economic class. According to [2], “the charitable sector, through the Misericórdias, took care of the poor, and liberal medicine took care of those who could pay” [1], thus highlighting their distinction between audiences.
With the progress of attention to health contributions, the government began to mention this aspect of health care. The economic data that was based on this government change was extracted from the Retirement and Pension Institutes.
Despite establishing access to health care as a right for everyone, until a social right was actually established, there were several changes and struggles in favor of equal rights. Despite the officialization of the public health body as part of the Federal Constitution of 1988, before this process there were changes in standards and guidelines in favor of this universalization of access and guarantee of health care.
According to [3], based on the ideas of [4], based on the assumptions that the universality of health is a guarantee of access for all to health facilities, regardless of their denomination, the entire population has the right to access conditions that enable stability in the health area.
The movement arising from the universalization of health is a federal projection tool, of states, municipalities, however, the execution comes from the entities closest to the regions, in short, the municipalities and states, with the federal sector being responsible for controlling and supervising the data [3].
Just as management takes place through these three sectors, the economy expected for the movement of the SUS region consists of this integration, as sanctioned Barbosa:
- In the budget structure, resources allocated to health come mainly from contributions on revenue and net profit, but Constitutional Amendment nº 29 also established a percentage of tax revenues collected by Municipalities (at least 15%) and States (at least 12 %) [3].
However, following studies and debates, it is already observed that such distribution is not done correctly, as the percentages to be contributed are not respected, allocating a lower amount to health bodies, which present damage in terms of the viability of purchase and production through this economic quantity to be deposited.
Given the research carried out in 2013, by Barbosa, regarding the list of municipalities when contributing to health bodies, only six made quotations at the rate required by law, namely: Amazonas, Pernambuco, Acre, Tocantins, Ceará and Rio Grande do Norte, while the others States reached a percentage of 11% to 8% in contributions to health alone.
The promotion of SUS as access to health for the entire population brought a new awareness regarding illnesses and care for the individual. Access occurred through consultations, vaccinations, treatments, prenatal care, among other achievements of access for all and rights provided by the state and municipalities.
In addition to these achievements, [3] highlights the expected improvements, as “the SUS has brought gains in terms of productivity in actions and services and in the population's health condition, which perhaps constitutes the ultimate objective of implementing a public health system” [3].
There were several modifications in order to highlight improvements regarding the population's access to health. In 2006, the Health Pact was established with visibility in three fundamental aspects:
- Health priorities to produce impacts on the population's health situation, explicit in the Pact for Life; 2) the general responsibilities in the management of the SUS, described in the Management Pact; 3) the commitments between managers with the consolidation of the Health Reform, proposing the expansion of dialogue with society in defense of the right to health and the SUS as a State policy, listed in the Pact in Defense of the SUS [3].
Even with many progresses, the SUS still constitutes a channel for improvement, whether in the service sector, in the financial areas, or in the transposition of its public service tools. In this condition, it is assumed that several changes will occur in favor of these improvements, thus establishing healthcare that is accessible to all, with quality and care, promoting even greater adherence on the part of the population when it comes to self-care.
Current Public Health Policies
In the historical process of the health area, it can be observed that society did not view this area as a primary issue in terms of serving the population, thus, health was always in the third place when it comes to the economic involvement of the country.
The right to health is a fundamental right, a type of social right, guaranteed to everyone by the Brazilian Federal Constitution. This is what can be extracted from the reading of article 6 of the 1988 Charter, the wording of which is stated as follows: “Social rights are education, health, food, work, housing, leisure, security, social security, protection of motherhood and childhood, assistance to the helpless, in the form of this Constitution” [5]. The constitutional text also contains, in article 196, the following provision:
- Art. 196 Health is the right of all and the duty of the State, guaranteed through social and economic policies that aim to reduce the risk of disease and other injuries and universal and equal access to actions and services for their promotion, protection and recovery [5].
It is a fact that the legislator's clear intention was to guarantee a minimum of dignity to the citizen, obliging the State to act in order to favor the reduction of the risk of diseases and other illnesses, also guaranteeing equal and universal access to services and actions aimed at your physical and mental well-being.
In compliance with this command, the Presidential Decree of March 13, 2006 established, within the scope of the Ministry of Health, the Commission on Social Determinants of Health (CNDSS), with the following objectives:
-
Support and articulate the actions of the Public Power, research institutions and civil society on social determinants related to improving health and reducing health inequities.
-
Promote effective models and practices related to the social determinants of health and aimed at including health equity in government policies.
-
Contribute to the formulation and implementation of health policies, plans and programs based on interventions on the social determinants that condition the level of health.
-
Organize and generate information and knowledge aimed at informing policies and actions on the social determinants of health.
-
Mobilize government sectors and civil society to act in the prevention and solution of the negative effects of social determinants of health [6].
Important functions were delegated to this commission, expressed in the objectives of its operation, outlined above. According to [7], its recognition expressed by the Head of Government (Federal President) that health is a public good, the construction of which must occur with the joint participation of all sectors of the Brazilian Company.
Also in this sense, this is the lesson given by [8], although it has long been known that health-disease is produced and distributed in society through strong processes of determination, both economic, social, environmental, political, cultural, etc., it is only in more recent times that this concept has experienced its incorporation into the practical and conceptual framework for formulating strategies and policies aimed at health.
According to the author, since 2003, the year in which the Global Commission on Social Determinants of Health was created, a process of systematization of available knowledge began, with the articulation of initiatives around the world, encouraging the formulation of policies based on of this structure. Immediately, this situation represented an expansion of the health field, with the strengthening of intersectoral approaches to health actions and policies - as happened in Brazil.
According to the CNDSS, SAD (Home care service) are factors that influence the appearance of health problems and risk factors identified in the population. Such factors, according to the Commission, include economic, social, ethnic/racial, cultural, behavioral and psychological factors.
For the World Health Organization (WHO), the Social Determinants of Health (DSS) correspond to the social conditions in which people work and live [7,9], on the other hand, it interprets them as social characteristics in whose life happens. [10], in turn, believes that it is possible to define SAD (Home care service) as elements of intervention, as they reveal mechanisms and factors through which social conditions affect health, potentially being changed by informative actions.
For [8], however, the importance should not be attributed to all determinants. This is because, among them, those that cause social stratification stand out. In this way, the most relevant DSS (Social Determinants of Health) are the structural ones, which reflect the conditions of distribution of power, wealth and prestige in the social context, and are therefore linked to income distribution, the structure of social classes and prejudice due to factors such as ethnicity, gender or disability and governance and policy structures that have fueled inequalities related to economic power rather than reducing it.
Among the mechanisms capable of generating and maintaining this stratification are the distribution of power between social classes, the ownership structures of the means of production and the institutions of informal and formal government. Educational systems, product and labor market structures can also be considered in this way; financial systems, revealing the level of attention given to distributional considerations as part of the policy-making process; and the nature and extent of redistributive, social protection and social security policies.
These structural mechanisms, according to Carvalho (2013), have the ability to change the social position of individuals, also revealing themselves as the main causes of health inequalities. They are, therefore, in his view, differences that, due to the impact they produce on intermediate determinants, such as biological and/or behavioral factors, psychosocial circumstances and living conditions, in addition to the health system itself, are responsible for shaping health by conditions of the individuals.
According to [7], it is necessary to consider that some health determinants are biological or are in a state in which the individual has greater control, as occurs, for example, with certain individual behaviors. Others, on the other hand, according to the authors, have collective coverage, which depends, for comparison, on existing social, political, economic, cultural and environmental conditions, as well as public and extra-sectoral health policies. Therefore, taking these assumptions into account, for the authors, action focused on SAD (Home care service) is necessary, which, in turn, encompasses both personal and external factors. Only in this way, in his opinion, could health be achieved.
Public health policy in the current decade, for its implementation, demarcated several legal and social changes to establish a condition of access for all, as mentioned in the previous topic. One of the contributions that consolidated the change in the health system was the indignation regarding health at the time, as expressed [11]:
- This Movement denounced the effects of the capitalist economic model on the health of the population and the irrationality of the health system then implemented. However, in addition to complaints, the Movement also presented alternatives for health reform, a project to change the current health system [11].
The process of access for all is reinforced by public policies that enable everyone, indiscriminately, to have access to viable health conditions for any issue. According to [11]:
- In the current situation, public policies provide efficient instruments in regulating and legitimizing “excluding universalization” through a system of segmented inclusion considered as citizenship, through openness to private initiative, targeting and selectivity [11].
This movement was adopted after the Federal Constitution of 1998 [5] which defined the process of consultation with the entire population free from any exclusion in the context of access to health care. In this way, it provided treatments, vaccinations, follow-ups, among others.
In relation to aspects of public health policies, these are defined by measures, proposals and actions provided by federal, state or municipal bodies regarding access and permanence in the context of care and assistance in the health area. Society, as the main individual who benefits from these public policy proposals, in short, should establish as a condition their participation in the process of choosing and developing these proposals, which aim to serve their class.
Despite its positive aspects in caring for the population, the political projections linked to the SUS present their challenges both in their constitution and in their continuity, as pointed out [12]:
- Underfunding, that is, the resources allocated to the operationalization and financing of the SUS, falls far short of its needs […] The insufficiencies of the local management of the SUS. The municipal management of SUS resources has only been working partially – without disregarding the fact that resources for the SUS are insufficient […] The low resolution of the basic service network set up in the country since the 1980s, but accelerated in the 1990s, as a result of disqualified care management, in particular due to the creation of a degraded clinic, the low capacity for building bonds and producing autonomy of users […] Deficiency in the training of health professionals […] Deficiency in the management of locoregional health systems [12].
Among the possibilities for changes to combat these conditions, the authors mention the Pact for Health, which promotes improvements and reforms in order to once again enhance the population's access and adherence to aspects linked to health. As provided:
- The pact introduced changes in relations between federated entities, including financing mechanisms, meaning, therefore, an effort to update and improve the SUS. For managers to adhere to the pact, a term of commitment is signed, in which commitments are established between managers in three dimensions: Pact for Life, in Defense of the SUS and Management [12].
There is a new health model, arising from Industry 4.0, called Digital Health - or Health 4.0. The replication of the principles of Industry 4.0 is affirmed in the incorporation of the digitalization of laboratory, medical and clinical data, as well as in the implementation of the mechanization of different manual processes that are currently applied in hospital environments and in healthcare in general [13].
Health 4.0 is a modern concept, created from concepts imagined around the world in Industry 4.0, which uses principles such as the Internet of Things (IoT) and cloud computing to promote transformations in processes, making them more agile and efficient. It is, therefore, a concept built on the basis of a progressive technological revolution, which began between 1760 and 1830, and which is currently in its fourth phase [14].
One of the possibilities with Health 4.0 is to consider the supply chain, to which the classification of cost centers has been attributed, as an opportunity for innovation, as through it, it will be possible to understand, with greater agility, the needs attributed to the end user. All this without leaving aside regional specificities, considered aspects of great importance in a country with the dimensions and complexities that Brazil presents [13,15].
Another aspect to consider is that, with Health 4.0, it is possible to expand the possibilities of collaborative partnerships between actors in the same value chain. This means they will be able to share coordinated production and distribution planning with each other in order to meet user needs more efficiently and quickly. This translates, therefore, into the idea of maintaining stocks adequate to the registered demand, in order to avoid unavailability of the product and/or delays in its supply [14].
Quality In Public Health
Quality is defined in the health sector, especially in hospitals, as the ability to manage people with guaranteed satisfactory levels of professional qualification, linked to the use and adequate control of technological resources, with the purpose of ensuring, for the client, an effective and low-risk treatment [16].
Currently, the excellence of health services is a target of concern and investment on the part of managers, bringing to the fore the discussion of quality and evaluation. From then on, the processes of improving health work, related to the search for quality, must be continuous and satisfy the needs of the patient [17].
From 1913, the premises of quality management in health services were strongly developed and systematized by the North American surgeon Ernest A. Codman [18]. This specialist limited his work to the idea of quality linked to the final product of the assistance provided [19].
The idea of Codman was strengthened around 1918, in the United States of America (USA), when members of the American College of Surgeons (CAC) developed the Hospital Standardization Program (PPH), through which the minimum standards to be achieved for quality assurance. However, this program was restricted to evaluating the results of medical procedures and work processes, not considering other aspects involved, such as customer satisfaction and structural conditions [18].
From the 1960s, the quality movement gained even more strength in the health area, with emphasis on Avedis Donabedian, an Armenian pediatrician, who elaborated important considerations regarding quality management models. Initially, Donabedian directed his studies to the quality of medical work and, soon after, broadened his perspective and began to involve other aspects of health services [20].
In your studies, Donabedian presented quality determined by three interdependent aspects, namely technical-scientific knowledge, interpersonal relationships and environmental factors. Soon after, it expanded its concept and developed the “Seven Pillars of Quality”: a) Efficiency; best result, in the best possible situation; b) Effectiveness: best result, in the best real situation; c) Efficiency: better result, with lower cost; d) Optimization: optimal point, considering results and costs; e) Acceptability: level at which the action meets the user’s expectations and values; f) Legitimacy: level at which the action meets society’s expectations and values; and g) Equity: level of distribution of shares among members of the population [21].
From the 1980s, quality control based strictly on the final result began to fail to meet the needs of services and the population. Given this, in 1988, Donabedian presented a new systematization for health quality, based on three management variables: structure, process and results of health care, where the structure encompasses physical, material, human, financial resources and organizational structure; the process, the care activities that involve health professionals and users, based on pre-established and accepted standards; and results, quality measures at the end of the treatment received, customer expectations and satisfaction [21].
These quality parameters have been successfully implemented in private hospital institutions, however, in the SUS, the reality is different. Aiming at a higher quality of health services provided by the SUS in Brazil, the National Hospital Services Assessment Program (PNASH) was created in 1998, which, in addition to applying a technical guide, develops user satisfaction surveys in urgency and emergency units, outpatient clinics and inpatient sectors, classifying institutions into five levels of quality, which are terrible, bad, regular, good and excellent. This program is used by public and private hospitals that are linked to the Single Health System (SUS). In 2004, faced with the need to expand its operationalization to other health services, PNASH was transformed into the National Health Services Assessment Program (PNASS) [22].
However, there are constant comments in the media on the subject of quality of health care, with the majority of clients and users of health services being dissatisfied. The need to guarantee positive results and satisfied customers in a competitive market requires quality in the way we operate.
The importance of quality in health was highlighted by the globalization process that brought new technologies and changes in political and socioeconomic scenarios, but imposed on managers the constant challenge of seeking tools and strategies to ensure excellence in services [23].
Furthermore, concern has increased with customer satisfaction who, over time, have become more informed, aware of their rights and able to choose and compare services [24].
This constant need to improve the quality of services reveals the complexity of health care and the need for a management system aimed at improving care and safety, using evaluation methods that allow demonstrating the efficiency and effectiveness of services. and the security provided to users [25].
The SUS is made up of a range of health actions and services that are provided by federal, state and municipal bodies based on the principles of universality, equity and comprehensiveness. After the decentralization of the SUS, it became easier to understand the particularities of each region in terms of its social, political and administrative reality [26].
The health sector has undergone transformations in the reconfiguration of care actions. Universality in care, the adoption of health policies based on the economy of supply and the difficulties in carrying out controls and establishing adequate regulatory mechanisms have reflected in the quality of services provided [27].
Vacancies Regulation Center
The SUS Vacancies Regulation Center plays a crucial role in the organization and distribution of health services in Brazil. This is a strategic mechanism that seeks to promote greater efficiency, transparency and equity in access to the different levels of medical care available in the country's public health system [28].
One of the main objectives of the Vacancies Regulation Center is to establish clear criteria for screening and classifying patients, considering the severity and urgency of each case. This approach is fundamental to optimizing the use of available resources, directing them more appropriately to those who need them most, thus reducing the wait for specialized procedures or treatments.
Allocating vacancies is a complex task, as it involves reconciling the growing demand for health services with the limitations of existing resources. However, the Center seeks to balance this equation, considering not only the urgency of the cases, but also regionalization criteria, so that care is distributed more fairly and equitably [29].
Another crucial point is monitoring and controlling the flow of patients and vacancies. Through systematic monitoring, the Center can identify bottlenecks and possible failures in the process, allowing adjustments and continuous improvements. This control also contributes to the transparency of the system, as citizens are able to monitor the progress of their requests and check the availability of vacancies.
Despite the efforts of the Vacancies Regulation Center, it is important to recognize that there are still challenges to be overcome. The high demand for healthcare services, the scarcity of resources in some regions and the complexity of the system can often lead to long waiting times for certain procedures. This reality makes the search for investments and improvements in SUS infrastructure and management essential [30].
Furthermore, it is essential that society as a whole engages in strengthening the public health system, understanding the importance of prevention and the search for a healthier lifestyle. Measures such as adopting healthy habits, regular access to primary care services and combating waste of resources can contribute to alleviating pressure on the Vacancies Regulation Center and, consequently, improving the supply and access to health services [31].
Operating within the scope of highly complex services (namely, tertiary care), the Bed and Admissions Regulation Center exercises its duties by regulating the allocation of hospital beds in health units affiliated with the SUS. This entity was created as a way to effectively manage the interaction between healthcare providers and patients and fulfills this objective by supervising the entire bed allocation process [29].
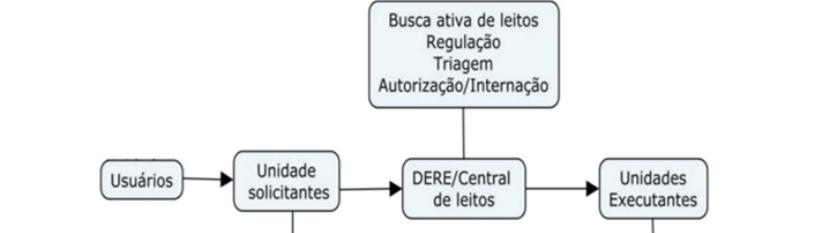
With regard to the availability of hospital beds linked to the SUS, the Bed and Admissions Regulation Center acts in accordance with its duties. Each entity involved in the process has a specific role to play. Thus, the regulation process is composed of three main components: the requesting units, which serve as the initial point of contact within the system; the regulation center, which facilitates the connection between the patient and the health unit; and, finally, the executing unit, belonging to the health establishment responsible for providing hospitalization services [29]. The user receives specialized assistance and guidance (Figure 1).
Figure 1: Flow of the hospital bed access regulation process.
The process begins with the completion of a report known as Hospital Admission Authorization (AIH) by the unit responsible for the request. This report is completed when a patient requiring medical care, hospitalization or emergency treatment is admitted to the requesting unit. Subsequently, the next step involves registering the patient in the Online Regulation System (SISREG), which generates a unique code upon registration, serving as confirmation that the patient was registered successfully. When entering the virtual queue, the patient will wait for each available space while their registration is pending.
The units responsible for health, such as basic units, specialized centers, hospitals and municipal health departments, play a fundamental role in this process. One of its main responsibilities is to register patients in the SISREG system and facilitate the transfer of patients to SUS hospital beds, when necessary.
Access to the Health Procedure Scheduling Tool: SISREG
Access to the health procedure scheduling tool, known as SISREG (National Regulation System), is an extremely important topic in the context of the SUS. It is a digital platform that aims to organize and optimize the scheduling of consultations, exams and specialized surgeries, seeking to provide greater efficiency and equity in access to health services [28].
The Ministry of Health developed SISREG, taking inspiration from the SOA-SUS Barreira initiative. This was done in accordance with Ordinance No. 1,559, of August 1, 2008. Article 1 of the ordinance determines the establishment of the National Policy for Regulation of the Single Health System (SUS). The policy must be implemented in all states, also respecting the jurisdiction of the three levels of government. SISREG serves as a tool to facilitate compliance with health-related obligations assumed by the respective government bodies [32].
In a country of continental dimensions like Brazil, ensuring access to healthcare procedures in an agile and fair manner is a significant challenge. SISREG appears as a response to this demand, seeking to standardize the flow of scheduling procedures, as well as facilitating the monitoring and monitoring of services [29].
One of the main advantages of SISREG is the possibility of centralizing information in a single system, which allows greater integration between different levels of health care. By sharing data, it is possible to avoid duplication of exams, speed up patient referral and ensure better coordination of care, especially when dealing with more complex cases that require the collaboration of different specialties [30].
Another important benefit is the transparency provided by the system. Both healthcare professionals and patients have access to information about scheduling and availability of vacancies, which contributes to reducing waiting lists and monitoring compliance with established deadlines.
However, despite the advances that SISREG has brought to the health system, there are still challenges to be faced. The computerization of scheduling can create difficulties for people with less access to technology or little familiarity with the use of digital systems. Furthermore, the lack of infrastructure in some regions of the country may limit the tool's full functioning, compromising its effectiveness.
Another point to be considered is the continuous need for system improvement. It is essential that there are investments in professional training, technological updates and improvement of processes to ensure that SISREG operates efficiently and fully meets the needs of the population [31].
For SISREG to fully fulfill its purpose of promoting fairer and more efficient access to healthcare procedures, a joint commitment is needed between managers, healthcare professionals and society in general. Continuous system improvement requires a broad view of demands and collaborative work to overcome challenges that arise along the way.
Vacancies Regulation Center and Your Rights
The SUS Vacancies Regulation Center is an extremely relevant topic for legal analysis, as it involves issues related to access to health, equity, transparency and efficiency of the Brazilian public health system [28].
Firstly, it is important to highlight that the creation and operation of the SUS Vacancies Regulation Center are based on legal provisions provided for in the Federal Constitution of 1988 and the Organic Health Law (Law nº 8,080/1990). These laws establish the right to health as a duty of the State, with the State being responsible for promoting actions aimed at guaranteeing universal and equal access to health services [30].
In this context, the SUS Vacancies Regulation Center plays an essential role in organizing and distributing specialized health services according to criteria of priority and severity of cases, seeking to meet the population's demand in a fair and equitable manner [29].
However, the legal analysis of the SUS Vacancies Regulation Center must consider some challenges faced by the system. Among them, we can highlight the delay in care and the wait for specialized procedures, which can be interpreted as a violation of the constitutional principle of the reasonable duration of the process (article 5, LXXVIII, Federal Constitution), which also applies to the health field.
Furthermore, the legal analysis of the SUS Vacancies Regulation Center must consider the principle of efficiency, provided for in article 37 of the Federal Constitution. Therefore, it is important to check whether the system management is being carried out efficiently and whether measures are being adopted to reduce waiting times and optimize the distribution of available resources.
Another relevant point is the issue of transparency. The legal analysis must verify whether information on the availability of vacancies, screening criteria and the progress of procedures scheduling processes are being made available in a clear and accessible way to citizens, guaranteeing the right to information provided for in the Constitution (article 5, LXXVIII, Federal Constitution) [31].
Society's participation is also an important aspect in the legal analysis of the SUS Vacancies Regulation Center. It is essential that the population has effective mechanisms to present their demands, make complaints and monitor the Central's actions, thus promoting social control over the health system.
Among the challenges faced by the SUS Vacancies Regulation Center, it is also relevant to address the issue of the judicialization of health. Delays in care, lack of access to certain procedures or denial of specialized medical services have led many citizens to seek a solution to their health problems through legal action.
The judicialization of health highlights the need for a more in-depth legal analysis of public health policies and the management of the Vacancies Regulation Center. It is necessary to assess whether the priority and screening criteria are being applied appropriately, whether resources are properly used and whether the population's demands are being met in a timely manner.
Another point that deserves to be highlighted in the legal analysis is the responsibility of the State and health system managers. The right to health is a fundamental right guaranteed by the Constitution, and it is up to the State to guarantee its implementation. Therefore, the SUS Vacancies Regulation Center must be managed responsibly, always aiming for the well-being and dignity of citizens.
The legal analysis can also focus on the management and governance issues of the SUS Vacancies Regulation Center. Transparency in resource allocation, accountability and efficiency in service management are crucial aspects for improving the health system.
To advance the improvement of the SUS Vacancies Regulation Center, it is essential to encourage dialogue between the different actors involved, including managers, health professionals, users and civil society. Legal analysis can provide support for the development of more effective public policies that promote universal and equal access to health [31].
It is important to highlight that the SUS Vacancies Regulation Center is a fundamental piece within the Brazilian health system. Its role is to organize and distribute specialized services in a fair and efficient way. However, for the SUS to reach its full potential, it is necessary to face the challenges and ensure that health policies are in accordance with constitutional principles and current legislation.
Conclusion
The SUS Vacancies Regulation Center is a key element in organizing and optimizing access to specialized health services in Brazil. Its legal analysis is fundamental to ensure that the system operates in accordance with the constitutional principles of universality, completeness and equity, ensuring the right to health for all Brazilian citizens.
Through legal analysis, it is possible to identify challenges faced by the Center, such as delays in service, the judicialization of health and the lack of transparency. This critical assessment can provide support to improve system management, promote efficiency in resource allocation and ensure compliance with established deadlines.
Furthermore, it is essential to encourage society's involvement in supervision and participation in the health system. Social control is a powerful tool to promote the continuous improvement of the SUS, seeking joint solutions to challenges and ensuring that public policies are aligned with the needs of the population.
Finally, it is the State's responsibility to promote adequate investments in public health, strengthening the SUS as a whole. Only with the joint commitment of managers, health professionals and civil society will it be possible to achieve the SUS's main objective: to provide quality and accessible healthcare for all Brazilians, building a fairer, more inclusive and healthier society. The SUS Vacancies Regulation Center is one of the fundamental pieces in this journey, and its continuous improvement is essential for the Brazilian public health system to reach its full potential and be a reference for excellence in health care for the population.
References
- Gerschman S, Santos MAB. (2006) The Single Health System as an outcome of 20th century health policies. Br J Soc Sci. 21(61):177-90.
- Santos LAC. (2004) Power, ideology and health in Brazil in the First Republic: historical sociology essay. In: HOCHMAN, G.; ARMUS, D. (Orgs.). Caring, controlling, healing: historical essays on health and illness in Latin America and the Caribbean. Rio de Janeiro: FIOCRUZ Publishing Company. 249-93.
- Barbosa EC. (2013) 25 years of the single health system: achievements and challenges. Health Systems Management Magazine. 2(2):85-102.
- Vasconcelos CM, PASCHE DF. (2006) The Single Health System. In: CAMPOS, G. W. S.; BONFIM, J. R. A.; Minayo MCS, AKERMAN M, JÚNIOR MD, CARVALHO YM. (Orgs.) Collective Health Treaty. São Paulo: Hucitec. 531-562.
- https://www.planalto.gov.br/ccivil_03/constituicao/constituicao.htm. Accessed on: August 8, 2023.
- https://bvsms.saude.gov.br/bvs/saudelegis/gm/2006/prt0399_22_02_2006.html. Accessed on: August 8, 2023.
- Buss PM, Pellegrini Filho A. (2007) Health and its social determinants. Physis: Public Health Magazine. 17(1):77–93.
- Carvalho AI. (2013) Social, economic and environmental determinants of health. In: FUNDAÇÃO OSWALDO CRUZ. Health in Brazil in 2030 - strategic prospecting of the Brazilian health system: population and health profile. Rio de Janeiro: Fiocruz/Ipea/Ministry of Health/Secretariat of Strategic Affairs of the Presidency of the Republic. 19-38.
- Tarlov AR. (2008) Social Determinants of Health: the sociobiological translation. In: BLANE, D.; BRUNNER, E.; WILKINSON, R. Health and Social Organization: towards a Health Policy for the 21st Century. London: Routledge, 1996.Theodoro.
- Scliar M. (2007) History of the concept of health. Physis: Collective Health Magazine. 17(1)29-41.
- Moraes JSS. (2017) Health policy today: challenges to the consolidation of the SUS. In: Proceedings of the 7th National Front Against Health Privatization Seminar, Maceió, Alagoas.
- http://sms.sp.bvs.br/lildbi/docsonline/get.php?id=5455. Accessed on: August 8, 2023.
- Malta DC, Reis AAC, Jaime PC, Morais Neto OL, Silva MMA, Akerman M. (2018) The SUS and the National Health Promotion Policy: perspective on results, advances and challenges in times of crisis. Science & Public Health. 23(6):1799-09.
- Franco G, Villardi JWR, Machado JMH, Souza MS, Brito IF, et al. (2017) Brazilian Health Surveillance: reflections and contribution to the debate at the 1st National Health Surveillance Conference. Science & Public Health. 22(10).
- Pinto LF, Rocha CMF. (2016) Innovations in Primary Health Care: the use of communication and information technology tools to support local management. Science & Public Health. 21(5):1433-48.
- Juliani CMCM, Kurcgant P. (2010) Continuing education and participant management: quality indicators of nursing human resources management. Science, Care and Health. 9(3):446-56.
- Saes AC. (2011) Consumer evaluation and satisfaction. In: HARADA, M. J. C. S. Nursing management: tool for safe practice – COREN. São Caetano do Sul: Yendis. 269-76.
- Ruthes RM, Alves VLS, Feldman LB, Cunha ICKO. (2011) Competencies in the quality scenario and the health manager. In: ALVES, V. L. S.; FELDMAN, L. B. (Orgs.). Health managers in the field of quality: performance and skills. São Paulo: Martinari. 21-27.
- Kaemmerer A. (2009) Safety in hospital care. GVSaúde Debates Magazine. 6:5-12.
- Manzo BF, Brito MJM, Corrêa AR. (2012) Implications of hospital accreditation on the everyday lives of healthcare professionals. USP Nursing School Magazine. 46(2):388-94.
- https://books.google.co.in/books/about/The_Definition_of_Quality_and_Approaches.html?id=G69pAAAAMAAJ&redir_esc=y
- https://bvsms.saude.gov.br/bvs/publicacoes/PNASS_programa_nacional_avaliacao_servicos_saude_2004_2005.pdf.
- http://hdl.handle.net/10174/3643
- Camelo SHH, Pinheiro A, Campos D, Oliveira TL. (2009) Nursing audit and the quality of health care: a literature review. Artigo. 11(4):1018-25.
- Treviso P, Brandão FH, Saitovitch D. (2009) Construction of indicators in health services. Health Administration Magazine. 11(45):182-86.
- Peron C. (2009) Audit and Management Agreement. Health Care Network Magazine. 3(3).
- Paim CRP, Ciconelli RM. (2007) Audit to assess the quality of health services. Health Administration Magazine. 9(36):85-92.
- Silva EL, Dutra KCS. (2015) The SUS Vacancy Regulation System: guaranteed access or bureaucratization of services? 2015. Course Completion Work (Graduation in Social Service) - School of Social Service, Federal University of Rio de Janeiro, Rio de Janeiro.
- Ramos U, Ramos W. (2017) Role of the bed regulation center of the Single Health System (SUS) in access to hospital admission services in the city of Belém, state of Pará. Biosphere Encyclopedia. 14(25):1570.
- Giovanella L, Rizzotto MLF. (2018) Primary Health Care: from the Alma-Ata Declaration to the Astana Charter. Health in Debate. 42(Spe1):6-8.
- Feitosa RMM, Paulino AA, Lima Júnior JOS, Oliveira KKD, Freitas RJM, et al. (2016) Changes offered by the National Program for Improving Access and Quality in Primary Care. Health and Society. 25(3):821-29.
- https://bvsms.saude.gov.br/bvs/saudelegis/gm/2008/prt1559_01_08_2008.html. Accessed on: August 8, 2023.

