Significance of Microbubble Contrast Study in Identification of Right Atrial Masses
Alekhya Abburu1*, Basharat Ahmad2, Prabakaran Gopalakrishnan3 and Ataul M. Qureshi4
1AA, MBBS graduate- Clinical Observer, Aultman Deuble Heart and Vascular Center, Canton, Ohio
2BA, MD - Clinical Fellow, Department of Cardiology, Aultman Deuble Heart and Vascular Center, Canton, Ohio
3PG, MD – Consultant Cardiologist, Department of Cardiology, Aultman Deuble Heart and Vascular Center, Canton, Ohio
4A M.Q, MD – Consultant Cardiologist, Department of Cardiology, Aultman Deuble Heart and Vascular Center, Canton, Ohio
*Corresponding author: Alekhya Abburu, AA, MBBS graduate- Clinical Observer, Aultman Deuble Heart and Vascular Center, Canton, Ohio
Citation: Abburu A, Ahmad B, Gopalakrishnan P, Qureshi AM. (2024) Significance of Microbubble Contrast Study in Identification of Right Atrial Masses. Adv Clin Med Res. 5(4):1-8.
Received: September 05, 2024 | Published: September 21, 2024
Copyright© 2024 genesis pub by Abburu A. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/ACMR.2024.5(4)-91
Abstract
Background: Cardiac masses are exceptionally rare but pose the most dangerous threat to the human body. They may be benign, malignant or tumor-like conditions such as thrombus or extracardiac cysts. The classification of these lesions is an important predictor of mortality. Several factors are considered helpful in establishing a diagnosis and treatment plan such as the location of the mass, age at presentation and imaging characteristics. Left atrium is the most common cardiac mass entity. However, a mass in the right atrium creates unique challenges because of the presence of normal anatomic variants that can mimic a tumor. Right atrial masses are rare and cannot be diagnosed unless a histopathological specimen is obtained. Here we present a case of a female, with two right atrial masses, highlighting the diagnostic challenges in arriving at a definitive diagnosis.
Methods and Result: A 39-year-old healthy female with no medical history presented with acute onset shortness of breath and palpitations. EKG showed new-onset atrial fibrillation with occasional premature ventricular complexes and clinically, she was in acute decompensated heart failure. She was scheduled for a direct current cardioversion and a transesophageal echocardiogram (TEE) was performed which revealed interesting findings of a large 3 cm mobile mass attached to the right atrial wall through a stalk and an underlying small mass of 1.5 x 0.9 cm. Furthermore, microbubble contrast media was utilized to assess the nature of the masses. Contrast-enhanced echocardiographic images presented uptake in the periphery of the large mass but no uptake otherwise. Using this technique, we detected a partially vascularized mass which later turned out to be a vascularized thrombus.
Conclusion: Most of the cardiac tumors are benign and cannot be differentiated from a vascularized thrombus. Echo contrast image enhancement by the ultrasound waves utilizing the echogenic properties of the microbubble contrast agents helps assess various vascularized cardiac structures and tumors, which are difficult to visualize on traditional ultrasound. Using this technique, we detected partially echocardiogenic contrast-enhanced masses that were later detected as an organized thrombus.
Keywords
Right atrial mass; Thrombus; Microbubble contrast study; Transesophageal echocardiogram (TEE).
Introduction
Microbubbles are developed for clinical molecular imaging. They are purely intravascular contrast particles with a diameter of several micrometers. Molecular imaging using microbubble-based ultrasound contrast agents is potentially useful in monitoring the biomarker status of vascular endothelium, enhancing the tumor vasculature and inflammation. It is also useful in detecting ischemia-reperfusion injury zones and thrombi [1]. The bubble surface is coated with suitable ligands that bind to target receptors on vascular endothelium, accumulating at the disease site. Echo from the targeted bubbles helps visualize the biomarker pattern. 90% of masses are either primary, originating from the pericardium or myocardium, or secondary due to malignancy [2]. It is important to differentiate the intracardiac mass as either a thrombus or a tumor. Although very uncommon, right atrial masses possess the same threat as left atrial masses. They may dislodge and cause serious life-threatening cerebral ischemia. A thorough diagnostic approach is required for timely interventions. The gold standard modality for diagnosing cardiac masses is Transesophageal echocardiography by using ultrasound-enhancing agents, which increases the accuracy and reliability of the said, leading to changes in treatment, improving patient outcomes and improving overall healthcare costs [3]. This case is an example of such Contrast-enhanced mass later found to be a thrombus with microbubble contrast study.
Case Presentation
39-year-old pleasant lady with no significant past medical history presented to the emergency department with complaints of shortness of breath and palpitations. Denies any chest pain, dizziness, PND, or orthopnea. She is not on any medications. She denies the use of tobacco, alcohol or illicit drugs. Family history is positive for atrial fibrillation in the mother. She eventually developed new-onset atrial fibrillation with rapid ventricular response and congestive heart failure. ProBNP was elevated, however cardiac biomarkers were normal. She was given 1 dose of digoxin, 1 dose of Lasix and startezmetoprolol. TEE showed a large right atrial mass measuring 2.6 x 2.9cm attached to the right atrial free wall (Figure 1).
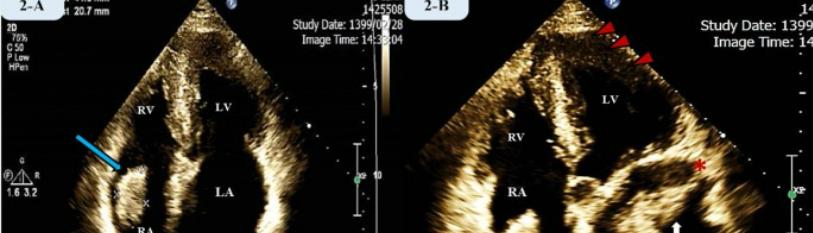
Figure 1: Transesophageal echocardiography showing right atrial masses.

There was also a smaller mass of 1.5 x 0.9cm underneath the larger one. Furthermore, microbubble contrast media was utilized which showed enhanced echocardiogenic images depicting uptake only in the periphery of the larger mass (Figure 2) sparing its central part and no enhancement in the smaller mass. Left Heart catheterization was performed to rule out any underlying coronary diseases, and showed normal RCA & LAD territories (Figure 3). TEE done before cardioversion showed no left atrial thrombus and a 2.6 x 2.9cm mass attached to the right atrium. She was hemodynamically stable with no pertinent findings on the physical exam. The patient was referred to a cardiothoracic surgeon for urgent resection.
Figure 2: 3D echocardiographic findings of right atrial mass showing microbubble contrast uptake in periphery.
Figure 3: Cardiac catheterization done prior to surgery, showing normal RCA and LAD
She was scheduled for an urgent open-heart surgery for resection of the atrial mass with primary closure of the atrial wall, pulmonary vein isolation using AtriCure and Compass radiofrequency system, and left atrial appendage occlusion.
Figure 4: Pathologic specimens of resected Right atrial mass showed organized thrombus.
After a successful operation, two masses were resected from the right atrial wall. Gross examination (Figure 4) revealed thrombi and microscopic analysis showed that the larger mass was an organized thrombus with peripheral vascularization. Postoperatively, she had bradycardia and was placed on a dobutamine drip. She developed small bilateral pleural effusions, which were treated subsequently. Later on, she developed a junctional rhythm (Figure 5) with a rate in 60s, and hence had an EP consult. She was placed on a 30-day Cardio Net monitor and was discharged with a follow-up request in 1-2 weeks.
Figure 5: Post-operative ECG revealing junctional rhythm.
Discussion
Myxomas account for 40-50% of primary cardiac tumors and have an estimated incidence of 0.0075%. Although the left atrial cavity may include up to 75-85% of myxomas, the right atrium also contains 25% of cases [4]. Unintentionally, atrial myxomas are frequently found in asymptomatic individuals. Right atrial masses present diagnostic challenges due to the broad spectrum of potential diseases. Intracardiac masses can be neoplastic or non-neoplastic [5]. A history of immobility and metastatic thrombi from peripheral deep veins are common in patients with right atrial thrombi. Intracardiac masses can occasionally be caused by malignancy [6]. Endothelial damage, hypercoagulability, and organic heart diseases such as right heart failure, atrial fibrillation, right atrial valve replacement, and pacemakers are the most frequent causes of right atrial thrombus [7,8]. In our patient, the possible cause is new-onset atrial fibrillation. Complications such as paradoxical migration over the foramen ovale or pulmonary embolism, which are significantly less common in right atrial appendage thrombi brought on by Afib, raise the risk of systemic embolization [9].
The incidence of thrombi in RAA is not well-documented. In 84.3% of adults, multilobed RAA (two lobes or more) is detected [10]. Transthoracic echocardiography is often used to diagnose cardiac mass, but it cannot determine the nature of the mass. Three forms of right heart thrombi were described and a morphological classification was proposed by the European Working Group on Echocardiography in 1989 [11]. The most prevalent kind of thrombi, known as type A thrombi, resemble serpiginous worms and are freely mobile within the heart chambers. They are also typically linked to pulmonary embolism and deep vein thrombosis. Type B thrombi are thought to originate in situ in connection with underlying cardiac problems. They are ovoid in shape, non-mobile, and firmly connected to the chamber wall. Lastly, type C thrombi are extremely mobile and uncommon and resemble atrial myxoma in appearance. This case resembled type C microthrombi and was initially considered an atrial myxoma.
Transesophageal echocardiography (TEE) improves the overall visualization of masses, particularly those in the posterior chamber [6]. It is quite uncommon for TEE to visualize right atrial thrombus when left atrial thrombus is absent, particularly in cases of AFib [12]. In our patient TEE with microbubble contrast was used to visualize the masses and differentiate the tumor from the thrombus. Microbubbles are employed as blood-pool agents in cardiology and radiology for contrast ultrasonography imaging [1]. Their potential as molecular imaging agents is gradually being acknowledged. It is possible to functionalize microbubbles with ligand molecules that attach to disease-related molecular markers. In carotid arteries, contrast-enhanced ultrasound can depict intraplaque neovascularization which correlates with plaque vulnerability [13] Microbubbles have clinical potential in perfusion imaging. Atrial fibrillation and flutter are among the most significant risk factors for thrombus development. The incidence of LAA and RAA thrombus in recent-onset tachyarrhythmias, according to Alberto et al., varied from 6-18% in AFib and 4-11% in Atrial flutter. Nonetheless, the study noted that compared to LAA, RAA thrombi are significantly less common.
Multiplane TEE is the sole predictor of RAA morphology and functional assessment [14]. It is extremely rare for right atrial thrombi to develop when Afib is present. This is because the right atrial appendage is much shallower than the left, which makes it less receptive to thrombus formation. Right atrial appendage thrombi are seen in patients with atrial fibrillation between 3% and 6% of the population, whereas left atrial thrombi affects 13% of the same patients [15]. The treatment of right atrial masses is determined by the patient's clinical status and the procedure's success rate. Many alternatives for treatment are put forward, including thrombolysis, embolectomy, and anticoagulation. According to Rose et al., individuals who got thrombolytic therapy had a reduced death rate in comparison to those who had anticoagulation or surgery. Thrombolysis is a safe treatment that breaks up clots in three main locations: intracardiac, pulmonary, and deep vein thrombosis and is safe to use in patients with contraindications to the other two treatment modalities [16] Since our patient had no existing comorbidities or pertinent physical findings, and considering her age, she was an ideal candidate for surgery.
Conclusion
Majority of patients with right atrial thrombi are asymptomatic, and get detected on routine cardiac evaluation. The presence of RAA thrombus is rare and an indication of potentially high-risk pulmonary embolism. Hence serial echocardiography is done to rule out any underlying causes of RAA thrombus. The use of contrast agents in echocardiography enhances the ability to differentiate between intra-cardiac thrombi and tumors. The echogenicity created by microbubble contrast agents leads to enhanced images by ultrasound waves which helps to correctly diagnose and treat the underlying condition.
Declarations
Abbreviations
None
Ethics Approval and Consent to Participate
NA
Consent for publication
Informed consent was obtained from the subject
Availability of data and material
Data is contained within the article
Competing interest
Authors declare no competing interests.
Funding
NA
Author contributions
All the authors have equal contribution in preparation of manuscript.
Acknowledgment
None
References
- Strachinaru M, Cate FJT. (2022) Microbubble Enhanced Echocardiography in Current Cardiology Practice. Re Cardiovasc Med. 23(6):202
- Jr HAM. (1979) Primary tumors and cysts of the heart and pericardium. Curr Probl Cardiol 4(2):1-51
- Dujardin KS, Click RL, Oh JK. (2000) The role of intraoperative transesophageal echocardiography in patients undergoing cardiac mass removal. Journal of the American Society of Echocardiography. J Am Soc Echocardiogr 13(12):1080-3.
- Rajani R, Nagaraja Sarangmath, Mishra B. (2008) Massive right atrial myxoma. International J Cardiol. 1:121-2.
- Kassop D, Donovan MS, Cheezum MK, Ngyen BT, Gambill NB. (2014) Curr Cardiovasc Imaging Rep 7(8):9281
- Lobo A, Lewis JF, Conti CR. (2000) Intracardiac masses detected by echocardiography: Case presentations and review of the literature. Clin Cardiol. 23(9): 702–708.
- Javanshir E, Sadat-Ebrahimi SR,Parvizi R, Parvizi R, Toufan M et al. (2019) Giant mass but small symptoms; huge thrombosis in the right atrium originating from the superior vena cava and protruding to the right ventricle. 13(1):312
- Lyon AR, López-Fernández T, Couch LS, Astggiano R. Aznar MC et al. (2022) ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio- Oncology Society (IC-OS). Eur Heart J. 43(41):4229-4361
- OMRAN H, JUNG W, MACCARTER D, et al. (2021) Right Atrial Thrombi and Depressed Right Atrial Appendage Function After Cardioversion of Atrial Fibrillation. J Investig Med High Impact Case Rep. 9: 23247096211010048
- Rissi R, Marques MJ, Neto HS. (2019) Checking the shape and lobation of the right atrial appendage in view of their clinical relevance. Anat Sci Int. 94(4):324-329
- KRONIK G. (1989) The European Cooperative Study on the clinical significance of right heart thrombi. Eur Heart J. 10(12):1046-59.
- Ozer O, Sari I, Davutoglu V. (2010) Right Atrial Appendage: Forgotten Part of the Heart in Atrial Fibrillation. Clin Appl Thromb Hemost. 16(2):218-20
- Feinstein SB. (2006) Contrast ultrasound imaging of the carotid artery vasa vasorum and atherosclerotic plaque neovascularization. J Am Coll Cardiol. 48(2):236-43.
- Cresti A, Ma GF, Gennaro Miracapillo, Miracapillo G, Picchi A et al. (2014) Frequency and Significance of Right Atrial Appendage Thrombi in Patients with Persistent Atrial Fibrillation or Atrial Flutter. J Am Soc Echocardiogr. 27(11):1200-7.
- Bashir M, Asher CR, Garcia MJ, Abdalla I, Jasper SE et al. (2001) Right atrial spontaneous echo contrast and thrombi in atrial fibrillation: a transesophageal echocardiography study. J Am Soc Echocardiogr. 14(2):122-7
- Shah CP, Thakur RK, Ip JH, Xie B, Guiraudon GM et al. (1996) Management of Mobile Right Atrial Thrombi: A Therapeutic Dilemma. J Card Surg. 11(6):428-31

