SASI Operation
Abdulrahman A Ashy1*, Ahmed A Abulnoor1, Yosra S Rezk1, Mosab I Saleh1 and Elhendawi M Abdelkhalek1
1Andalusia Hospital, Jeddah, Saudi Arabia
*Corresponding author: Abdulrahman A Ashy, Andalusia Hospital, Jeddah, Saudi Arabia.
Citation: Ashy AA, Abdulnoor AA, Rezk YS, Saleh MI, Abdelkhalek EM. (2023) SASI Operation. Genesis J Surg Med. 2(1):1-4.
Received: June 15, 2023 | Published: June 30, 2023
Copyright© 2023 genesis pub by Ashy AA, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/GJSM.2023.2(1)-14
Abstract
Obesity is becoming more and more increasing in incidence all over the world including our kingdom. Many trials were adopted to treat this disease from dieting and exercises up to the surgical intervention. The different procedures have their own advantages and disadvantages. Our own experience with the Single Anastomosis Sleeve Ileal (SASI) bypass will be discussed here with review of literatures.
Keywords
Sasi; Lsg; Roux-en-Y gastric bypass; Bariatric surgery
Introduction
Single anastomosis sleeve gastrectomy ileal bypass (SASI) is a procedure which combines the advantages and avoids the disadvantages of the gastric restrictive and the malnutritional ones. It decreases the postoperative incidence of leakage and heartburn as well as the need for long term nutrient supplementation by maintaining the passage of the food and drink through the normal channel of the digestive tract.
Aim of The Operation
SASI operation is a modified Omega loop gastric bypass. It has the advantages of both sleeve gastrectomy and gastric bypass by minimizing the size of the stomach and decreasing the appetite by removing the ghrelin hormone responsible for huger, as well as reducing the long-term complications of gastric bypass.
Material and Methods
Surgical Technique
Before surgery, the patient is sent to have the routine investigation done i.e. blood tests including serology and coagulation profile as well as chest x-ray & ECG, then sent to be seen and assessed preoperatively by the Anaesthetist. An informed consent is taken in the outpatient clinic.
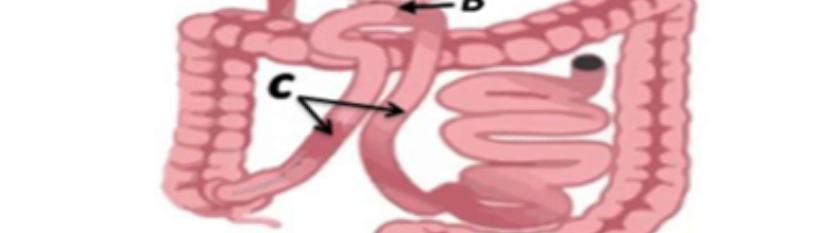
One day before surgery, the patient is advised to put himself or herself on liquid diet until midnight, and then to take only water up to two hours before starting the operation. IV antibiotic is given and the mechanical anti-thrombotic measure using the automatic inflatable bag is applied after giving the general anaesthesia with endo-trachial intubation. The patient is put on table supine in the French position and anti-Trendelinburg. The patient is draped and the abdominal cavity is insuflated with CO2 up to a pressure of 18mm mercury. Five ports are used. We start first by creating the sleeve gastrectomy. About 75%-80% of the stomach is resected and removed. Then a length of about 250cm from the ileocaecal junction is measured and connected to the antrum of the stomach as Omega loop using an endo-GIA stapler size 45 and the hole is closed with V-lock suture material [Figure 1]. The integrity of the staple line as well as the gastroileal anastomosis is tested with Methylene blue. Size 19 JVac suction drain is left around the stomach. The abdominal cavity is desuflated and the wounds are closed with rapide 3/0. The patient is encouraged to walk up & about after full recovery and allowed sips of water at night. On the following day of the operation, Gastrographin study is done and the patient is discharged home by the end of the same day to be seen in the outpatient clinic after one week, then after 3, 6 & 10 months [Figure 2] (1-6).
Advantages and disadvantages of the SASI
Results and Discussion
SASI operation was practiced since 2012. Many centres around the world have established their experience regarding this investigational procedure to improve the weight loss and comorbidities. we started practicing this operation since September 2022 on 14 patients of different nationality (5 males & 9 females). The original weight on admission ranges between 78 kg - 195 kg, and the BMI between 32.8 kg/m2 - 64.4 kg/m2. Their mean BMI after three months to ten months was 41 kg/m2 (average 27.83 - 54.5 kg/m2). The total weight loss after three months to ten months was 13.4% (12 kg) to 41.0% (80 kg) respectively among our patients. All our patients had complete remission of their type 2 diabetes (100%), hypertension (75%), sleep apnea (100%) and hyperlipidemia (89%). None of our patients complained of heart burn (reflux) or dumping syndrome and no vomiting or regurgitation.
Conclusion
As a result of our patient’s satisfaction and no complaints during the period of the first ten months after they were subjected to the SASI operation as well as the satisfactory results regarding the weight loss and remission of the comorbidities, we think that SASI will be a promising procedure in the treatment of patients suffering from morbid & super obesity in the future especially those who love sweets or suffer from gastroesophageal reflux, but it still needs more cases and long term follow up to ensure its efficacy in different centres.
References
- Mahdy T, Al wahedi A, Schou C. (2016) Efficacy of single anastomosis sleeve ileal (SASI) bypass for type-2 diabetic morbid obese patients: Gastric bipartition, a novel metabolic surgery procedure: A retrospective cohort study. Int J Surg. 34:28-34.
- Emile SH, Mahdy T, Schou C, Kramer M, Shikora S. (2021) Systematic review of the outcome of single-anastomosis sleeve ileal (SASI) bypass in treatment of morbid obesity with proportion meta-analysis of improvement in diabetes mellitus. Int J Surg. 92:106024.
- Attia N, Khlifa MBH, Fadhel NB. (2021) The single anastomosis sleeve ileal (SASI) bypass: A review of the current literature on outcomes and statistical results. Obes Med. 27:100370.
- Mahdy T, Emile SH, Madyan A, Schou C, Alwahidi A et al. Evaluation of the efficacy of Single Anastomosis Sleeve Ileal (SASI) Bypass for patients with Morbid Obesity: A Multicenter Study. Obes Surg. 30(3):837-45.
- Husseini SV, Moeinvaziri N, Medhati P, Salem SA, Hosseini E et al. (2022) The effect of Single-Anastomosis Sleeve Ileal (SASI) bypass on patients with severe obesity in Three Consecutive Years. World J Surg. 46(11):2744-50.
- Kamal A, El Azawy M, A. Hassan TA. (2023) Unpredictable Malnutrition and Short- Term Outcomes after Single Anastomosis Sleeve Ileal (SASI) bypass in Obese Patients. J Obes.

