Renal Complications Due to Breast Cancer
Leila Alem*
Isfahan University of Medical Sciences, Isfahan, Iran
*Corresponding Author: Leila Alem, Isfahan University of Medical Sciences, Isfahan, Iran
Citation: Alem L. Renal complications due to breast cancer. J Can Ther Res. 4(1):1-5.
Received: September 01, 2024 | Published: September 15, 2024
Copyright© 2024 genesis pub by Alem L. Yu, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non-Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JCTR.2024.4(1)-34
Abstract
Kidney disease frequently occurs among individuals diagnosed with cancer. Given the high incidence of comorbidities in patients treated for active malignancies, it is not surprising that these individuals often develop renal disease, which is common in other hospitalized patients. The function of the nephrologist in those instances differs little in phrases of presence or absence of cancer. On the other hand, cancer patients are characterized by several renal syndromes caused by the cancer itself or by its treatment. In addition, patients undergoing chemotherapy often require dialysis due to acute or chronic kidney disease.
Keywords
Breast cancer; Cancer; Acute renal failure; chronic kidney disease; Kidney dysfunction
Introduction
The most frequent non-dermatologic carcinoma in females is breast cancer [1], accounting for 23% of all women's cancers worldwide, with about 1.15 million patients detected in 2021. The highest incidence rates are observed in developed countries, while the lowest rates are found in developing countries like Africa, Asia, and the Middle East. The worldwide incidence of breast malignancy has risen by about 0.5% annually since 1990 (2). Breast carcinoma will be detected in 12% of females in the United States during their lifetimes and more than 250000 new sufferers have been identified inside the United States in 2017. More than 90% of breast carcinoma are not metastatic at the time of diagnosis. For non-metastatic cancer, the treatment goals are to eradicate the tumor and prevent recurrence [3].
Its common metastases include lungs, bones, lymph nodes, liver, and bladder. Less commonly, it affects the pancreas, spleen, kidney, adrenal glands, ovary, brain, thyroid, and heart. At the time of diagnosis, the majority of breast cancer patients had widespread illness. Poor prognosis is associated with metastatic disease, which typically occurs several years after diagnosis [1, 4]. It is possible that metastasis of breast cancer by extension into the renal vein results in a solitary renal mass, leading to a primary renal tumor. When a patient has breast cancer, a kidney histological investigation is recommended because appropriate, methodical treatment is preferable to nephrectomy in these situations [5]. Breast cancer has a relatively good prognosis; however, it ranks as the main reason for cancer death among females [6].
After 21 years, the survival of patients with breast cancer is similar to the expected survival of the general population. Eason and Russell showed that 18% of breast cancer patients may be cured of their disease [7]. The increased rate of acute kidney injury and chronic kidney disease between cases with cancer is concerning, particularly in persons with lung, colorectal, gynecological, prostate, and breast cancers. The association of cancer with kidney dysfunction worsens patient outcomes and complicates their management. Kidneys are an important place for drug elimination from the body, and as a result, they are exposed to high concentrations of chemotherapy drugs and their metabolites, which often cause nephrotoxicity [8, 9].
Acute renal failure is termed as a sudden decrease in glomerular filtration rate that causes an acute rise in blood urea nitrogen and serum creatinine [10]. It is a critical complication of cancer and the main source of morbidity and mortality. Studies show that acute renal failure can compromise the chances of cancer cases receiving optimum treatment. Acute renal failure may also be caused by causes resulting from cancer treatment or the disease itself, including post-renal obstruction, compression and invasion by malignancy, nephrotoxic chemotherapeutic agents, sepsis, tumor lysis syndrome, and contrast agent nephropathy [11]. Post-renal obstruction of acute renal failure in cancer cases is more common than in general people. Obstruction may happen anywhere in the genitourinary tract [12]. It is currently difficult to determine the exact incidence of acute renal failure in cancer patients due to different definitions of acute renal failure [13].
Acute kidney injury is a common incidence in cancer patients [14]. For example, in a study from Denmark of 1.2 million people, between 1999 and 2006, 37,267 cases of cancer occurred. In a year, 27% of cases advanced acute kidney injury, and 7.6% of cases developed severe acute kidney injury and acute kidney injury needing dialysis. In that investigation, the highest risk of acute kidney injury was between cases of kidney and liver cancer [15]. In a recent study of 163,071 cases that went through treatment for malignancy between 2007 and 2014, acute kidney injury that needed dialysis happened in nearly 10% of cases [16].
The rate of chronic kidney disease and its end-stage kidney disease is increasing in the population because of the lengthening of human life. A rise in the number of cases of end-stage kidney disease treated with kidney replacement is detected in the group 60 years old and older. Hemodialysis is the main technique of kidney replacement therapy [17]. The number of end-stage renal diseases is progressively increasing in Western countries, as well as in Asia [18]. The slow improvement in survival of patients treated with kidney replacement increases the chance of malignancy, causing a higher incidence of breast cancer [19, 20].
Chronic kidney disease is an independent risk factor for morbidity and mortality in multi-disease processes. Though, there is not much information about the relationship between chronic kidney disease and breast cancer [21]. Chronic kidney disease is an independent risk factor for the development of cardiovascular diseases and for many other disease developments [22].
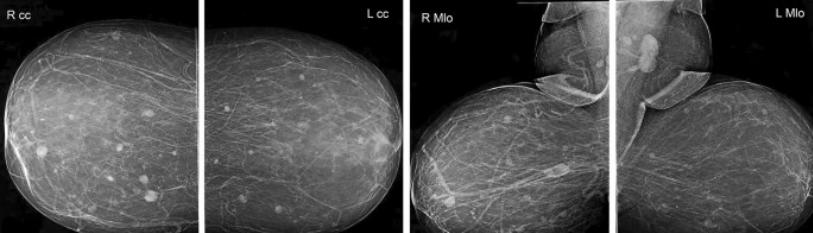
In cases with chronic kidney disease, patients can often have calcifications throughout their soft tissue. For this reason, females with chronic kidney disease have shown more calcification of their breast tissue compared to females without chronic kidney disease. Cases with Chronic kidney disease experience more breast biopsies. Conversely, they are also susceptible to delayed diagnosis [23].
A study of kidney failure and anticancer medications (IRMA) shows a high occurrence of abnormal kidney function in a population of 4684 solid tumor cases. As the patients and the medications used differ depending on the type of tumor, the IRMA study group began the analysis in several subgroups of patients. In IRMA cases with breast malignancy in 1898, the prevalence of renal insufficiency was still very high despite normal serum creatinine in most patients. Several anticancer medications, such as capecitabine, bisphosphonates, and platinum salts, may be nephrotoxic or require adjusting the dose. However, other main medications in breast cancer do not need dose reduction, and they have no kidney (trastuzumab, anthracyclines, taxanes) [24].
Treatment of breast cancer cases with Chronic kidney disease is complicated due to kidney dysfunction. Chemotherapy drugs are often cleared through the kidneys and can be nephrotoxic. Patients may experience nephrotoxic levels of their chemotherapy drugs. Moreover, patients may not be treated if the dosage of chemotherapeutics is modified due to fears of nephrotoxicity. Both of these can lead to reduced survival. Considering these factors, we imagined that Chronic kidney disease is an independent risk factor for mortality in breast cancer patients [21]. More than half of patients (52.9%) who started anticancer medication had kidney dysfunction and needed to adjust the dose of anticancer medications. However, the absence of appropriate drug dosage adjustment was associated with decreased overall survival.
The relationship between renal disease and cancer is complex and reciprocal. One of the most common renal diseases associated with cancer is electrolyte and acid-base disorders, which happen frequently and often have a poor prognosis, and acute kidney injury. Electrolyte and acid-base disorders are the result of neoplastic expansion, anticancer treatment, or, rarely, paraneoplastic phenomena of various tumors [25].
Acute kidney injury, continual renal failure, and tubular abnormalities constitute the kidney disorder spectrum of malignancy. Prompt prognosis and remedy might also additionally save you or opposite those complications. The pathogenesis of acute kidney harm in most cancers is multifactorial. Acute kidney injury affects outcomes in cancer, oncological therapy withdrawal, raised hospitalization rate, and hospital stay. Kidney feature derangement may be recovered with early detection and centered remedy of cancers. Finding instances of a better chance of renal harm and imposing preventive measures without sacrificing the advantages of oncological remedy enhance survival. Multidisciplinary approaches, together with relieving obstruction, hydration, etc., are used to reduce the renal damage rate.
Conclusion
Acute kidney injury, continual renal failure, and tubular abnormalities constitute the kidney disorder spectrum of malignancy. Prompt prognosis and remedy might also additionally save you or opposite those complications. The pathogenesis of acute kidney harm in most cancers is multifactorial. Acute kidney injury affects outcomes in cancer, oncological therapy withdrawal, raised hospitalization rate, and hospital stay. Kidney feature derangement may be recovered with early detection and centered remedy of cancers. Finding instances of a better chance of renal harm and imposing preventive measures without sacrificing the advantages of oncological remedy enhance survival. Multidisciplinary approaches, together with relieving obstruction, hydration, etc., are used to reduce the renal damage rate.

