Recurrent Primary Nocardia Brain Abscess (Nocardia farcinica) in an Immunocompetent Patient with a History of Non-Nocardial Multi-Systemic Infection
Mohammed Ali*, M. Heckelmann and CA Tschan
Krankenhaus Ludmillenstift, Department of Neurosurgery, Ludmillenstr. 4-6, 49716 Meppen, Germany
*Corresponding author. Ali M, Krankenhaus Ludmillenstift, Department of Neurosurgery, Ludmillenstr. 4-6, 49716 Meppen, Germany.
Citation: Ali M, Hackelmann M, Tschan CA, Recurrent Primary Nocardia Brain Abscess (Nocardia farcinica) in an Immunocompetent Patient with a History of Non-Nocardial Multi-Systemic Infection. J Neurol Sci Res. 4(2):1-6.
Received: November 18, 2024 | Published: December 4, 2024
Copyright©️ 2024 genesis pub by Ali M. et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non-Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: http://doi.org/10.52793/JNSRR.2024.4(2)-40
Abstract
Background: Nocardia species, particularly Nocardia farcinica, are rare causative agents of brain abscesses, with primary infections accounting for less than 2% of all brain abscesses. This report describes a unique case of a primary Nocardia farcinica brain abscess in an immunocompetent patient, highlighting diagnostic challenges and treatment outcomes.
Case Presentation
In this paper, we describe a case of an immunocompetent patient with cerebral nocardiosis. A 56-year-old male presented with a focal seizure affecting the right arm. Initial imaging revealed a well-defined contrast-enhanced lesion in the left occipital lobe. The patient was afebrile with no signs of sepsis, raising suspicion for metastatic disease.
His medical history included a recent right-sided hemicolectomy for suspected cecal carcinoma, although histopathological findings were negative for malignancy. Previous sputum cultures had identified Klebsiella pneumoniae and Candida albicans. After referral for neurosurgical evaluation, a biopsy of the brain lesion confirmed a Nocardia farcinica brain abscess. The patient was treated with intravenous linezolid, cotrimoxazole, and imipenem, followed by oral cotrimoxazole for a year. Despite initial improvement, he developed recurrent neurological symptoms, necessitating surgical excision and drainage of the abscess. Following an additional course of intravenous antibiotics, significant clinical and radiological improvement was observed.
Conclusion
Nocardia farcinica brain abscesses are rare but should not be excluded in the differential diagnosis of intracranial space-occupying lesions. Primary Nocardia brain infections can occur without evident immunosuppression or a clear primary source of infection. Multidisciplinary management, combining surgical excision and targeted antibiotic therapy, is essential for successful treatment. Long-term antibiotic therapy and close follow-up are crucial to prevent recurrence.
Keywords
Brain Abscess; immunocompetent patient; Candida albicans; linezolid; cotrimoxazole; imipenem; Brain Biopsy; Nocardia
Introduction
Nocardia is a Gram-positive aerobic filamentous bacterium, usually found in soil and water. Cerebral infections caused by Nocardia are rare and severe, usually presented as cerebral abscess in immunocompromised patients. The most common ways to acquire nocardial infection are inoculation and hematogenous spreading or inhalation [1-3].
Its diagnosis is difficult due to various symptoms caused by Nocardia, which mimic the true nature of the disease and result in a mortality rate of up to 60%. According to its pathognomonic nature, it is believed that hematogenous spreading from lung infection leads to cerebral involvement and subsequent brain abscess. Nocardia mimics multiple brain-related disorders, such as ischemic stroke, metastases, and primary brain tumors. Among the immunocompromised population, nocardiosis is most frequently an opportunistic infection that can result in both localized and systemic illnesses.
Primary brain abscesses caused by Nocardia species are exceedingly rare, accounting for less than 2% of all brain abscesses. Most cases are reported outside Europe. This report focuses on a unique case of a primary Nocardia farcinica brain abscess in an immunocompetent patient, detailing its clinical presentation, diagnostic challenges, treatment approach, and follow-up [4,5].
Case Presentation
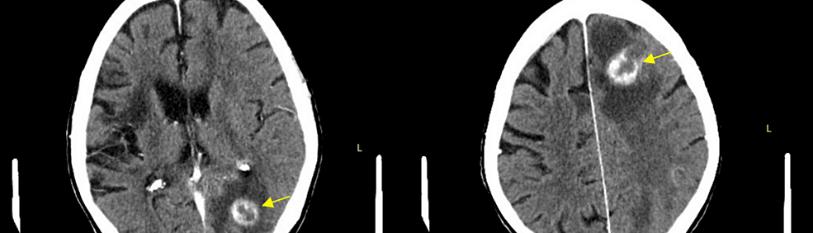
We describe the case of a 56-year-old male who presented with a focal seizure involving the right arm. Initial investigations at another hospital revealed a well-defined, contrast-enhanced, space-occupying lesion (13.5 × 7.8 mm) in the subcortical left occipital lobe on MRI. Referred to our neurosurgical department for further evaluation, the patient was afebrile and showed no signs of sepsis, leading to a differential diagnosis of metastatic tumor. CT scans of the thorax and abdomen were unremarkable. The patient’s medical history included a recent right-sided hemicolectomy with end-to-end anastomosis due to suspected cecal carcinoma. Although histopathology did not confirm malignancy, intraoperative smears identified Bacteroides vulgatus, and previous sputum cultures revealed Klebsiella pneumoniae and Candida albicans. The patient had completed a course of antibiotics prior to admission. A biopsy of the brain lesion confirmed a brain abscess caused by Nocardia farcinica. Treatment commenced immediately with linezolid, intravenous cotrimoxazole, and imipenem, followed by oral cotrimoxazole for one year. Despite initial improvement, the patient returned three days post-discharge with disorientation, impaired concentration, and aphasia. Repeated MRI Scan revealed a recurrent abscess, necessitating surgical excision and drainage. The patient received an additional four weeks of intravenous antibiotics and showed significant clinical and radiological improvement [6,7].
Treatment Regime
The treatment of the primary Nocardia farcinica brain abscess in this case involved a combination of surgical and medical interventions. Initially, the patient was started on a broad-spectrum antibiotic regimen, including linezolid, intravenous cotrimoxazole, and imipenem, due to their efficacy against Nocardia. This was followed by a prolonged course of oral cotrimoxazole for one year to ensure complete eradication of the infection [8-10].
Despite initial clinical improvement, the patient experienced a recurrence of neurological symptoms, which was confirmed by MRI as a recurrent abscess. As a result, surgical excision and drainage of the abscess were performed, which, combined with an additional four weeks of intravenous antibiotics, led to significant clinical and radiological improvement.
The treatment highlights the importance of both early surgical intervention and long-term antibiotic therapy in managing Nocardia brain abscesses. The success of the treatment regimen underscores the need for personalized management, particularly with respect to the selection of appropriate antibiotics based on Nocardia susceptibility.
Discussion
- Diagnostic challenges
Primary brain abscesses caused by Nocardia species are infrequently encountered, and their clinical presentation can overlap with other more common causes of brain abscesses, such as bacterial infections, fungal infections, and metastases. In this case, the patient’s initial presentation with a focal seizure and the MRI findings of a well-defined contrast-enhanced lesion raised suspicion for a metastatic tumor, which is a common differential diagnosis for space-occupying lesions in the brain. However, the absence of fever and signs of systemic infection, along with the patient’s lack of a known history of malignancy, prompted further investigation. One of the key challenges in diagnosing a Nocardia brain abscess is the difficulty in isolating the pathogen, as Nocardiaspecies are slow-growing and may not be readily identified in standard microbiological cultures. In this case, despite prior antibiotic therapy, the pathogen was ultimately identified through a biopsy of the brain lesion, confirming the diagnosis of Nocardia farcinica. This underscores the importance of considering rare pathogens like Nocardia when a brain abscess is suspected, particularly in the absence of clear predisposing factors.
2. Role of imaging
MRI played a crucial role in identifying the lesion and determining its location. Contrast-enhanced MRI is a sensitive modality for detecting brain abscesses, revealing well-circumscribed lesions with surrounding edema. While this can be suggestive of a brain abscess, the imaging findings are not pathognomonic for any single organism, as other causes, including metastases and abscesses from other bacterial or fungal pathogens, can appear similarly. Thus, MRI findings should always be interpreted in conjunction with clinical history, microbiological culture results, and surgical findings.
3. Treatment approach
The treatment of Nocardia brain abscesses typically involves a combination of surgical drainage and long-term antibiotic therapy. In this case, the patient was initially treated with intravenous linezolid, cotrimoxazole, and imipenem, reflecting the broad-spectrum approach often required in the initial stages of treatment for Nocardia infections. These antibiotics are effective against Nocardia species, which are inherently resistant to many common antibiotics, including beta-lactams. After initial improvement, the patient was switched to oral cotrimoxazole for long-term therapy, which is considered the cornerstone of treatment for most Nocardia infections.
However, despite the early improvement in symptoms, the patient experienced a recurrence of the abscess within days of discharge. This recurrence may be attributed to several factors, including the complexity of treating Nocardia infections, the difficulty in eradicating the pathogen, or incomplete resolution of the infection due to the brain abscess’s location or the patient’s prior antibiotic history. The need for surgical excision and drainage of the recurrent abscess, followed by an additional four weeks of intravenous antibiotics, emphasizes the importance of close monitoring and aggressive management in such cases.
4. Surgical management
Surgical intervention remains a critical component in the management of brain abscesses, particularly when there is a significant mass effect or if the abscess is inaccessible for medical management alone. In this case, despite the initial antibiotic treatment, the recurrence of the abscess required surgical drainage, which led to substantial clinical improvement. Surgical drainage helps reduce intracranial pressure, allows for the removal of infected tissue, and facilitates better penetration of antibiotics into the abscess cavity. Although surgical excision can be complicated by the lesion’s location and the risk of neurological deficits, it was essential for the patient’s recovery in this instance.
5. Prognosis and long-term management
The prognosis for Nocardia brain abscesses depends on several factors, including the patient’s immune status, the timeliness of diagnosis, and the effectiveness of surgical and medical interventions. In immunocompetent patients, like the one described here, the prognosis is generally more favorable, although recurrence can occur, as seen in this case. Long-term antibiotic therapy is essential to prevent relapse, and follow-up imaging is crucial to monitor for recurrence, as was done in this case. The patient’s significant clinical and radiological improvement after the second round of surgical and antibiotic treatment underscores the importance of early intervention and sustained therapy in achieving a favorable outcome.
6. Literature comparison
Reports of primary Nocardia brain abscesses are limited, with most cases occurring in immunocompromised patients, such as those with HIV, organ transplant recipients, or individuals on immunosuppressive therapy. This case is noteworthy for involving an immunocompetent patient, which makes it a rare occurrence in the literature. Similar to previous case reports, this patient’s diagnosis was delayed due to the atypical presentation, and initial treatment with broad-spectrum antibiotics was required. In contrast to many other cases, this patient’s abscess required surgical excision due to recurrence, which highlights the complexity of managing Nocardia brain abscesses even in patients with no obvious immune deficiencies.
Conclusion
This case highlights that a Nocardia brain abscess must be considered in the differential diagnosis of brain abscesses or space-occupying lesions, particularly in patients with a history of systemic or multi-systemic non- nocardia infections such as pneumonia, lung abscess, peritonitis, or gastrointestinal abscess. In my opinion, the Prompt diagnosis, surgical intervention, and tailored antibiotic therapy with regular Follow-Up for at Least One Year are critical to achieving a favorable outcome.
Ethics approval and Consent to Participate
All procedures performed in the study involving human participants were in accordance with the ethical standards of the Ethics Committee.
Consent for publication
Written informed consent was obtained from the individual, for the publication of any potentially identifiable images or data included in this article.
Competing Interests
The authors declare no competing interests.
References
- Chuang YC, Lin WC. (2001) Nocardial brain abscesses in immunocompetent patients: A report of four cases and review of the literature. Journal of Clinical Neuroscience, 8(1):35-40.
- Gavalda J, Sanclemente G. (2013) Central nervous system nocardiosis: Diagnosis and treatment. Clinical Microbiology and nfection, 19(5):438-42.
- Huang WC, Hsu CW. (2015) Nocardia farcinica brain abscess: A rare but treatable infection in immunocompetent patients. Journal of Infection and Chemotherapy, 21(6): 429-33.
- Leimgruber M, Manz M. (2010). Nocardia brain abscess: A case report and review of the literature. Clinical Infectious Diseases, 51(8): 931-37.
- Mylonakis E, Barlis P. (2002). Nocardial brain abscesses: Diagnosis and management. Clinical Infectious Diseases, 34(4):335-41.
- Taj-Aldeen SJ, Al-Mohsen IZ. (2012) Nocardia farcinica: A rare cause of brain abscess in an immunocompetent patient. The Journal of Infection in Developing Countries, 6(4):299-303.
- Wilson J W. (2012) Nocardiosis: Update on clinical manifestations, diagnosis, and treatment. American Journal of Medical Sciences, 343(3): 241-47.
- Wootton SH, Whittle BJ. (2006) Management of brain abscesses caused by Nocardia species: A clinical study. Journal of Antimicrobial Chemotherapy, 58(2):321-24.
- Zhao Y, Liu Q. (2016) Nocardia brain abscess: Clinical features and management strategies. Infection and Drug Resistance, 9:217-25.
- Zintgraff J, Prieto M, PeñaM, F, Simoiz F, Rosenblit S, et al.(2020) When reporting Nocardia spp is not enough Brain abscess caused by Nocardia farcinica. Access Microbiol, 2(2):acmi000091.
- Kim S, Lee KL , Lee DM , Jeong JH , Moon SM, et al. (2014) Nocardia Brain Abscess in an Immunocompetent Patient. Infect Chemother, 46(1):45–49.
- Koruga, Reljac G, Rončević A. (2014) Nocardia Brain Abscess in an Immunocompetent Patient. Infect chemother.46(1):45-9.
- Koruga N, Reljac G, Bogdan M, Sabadi D, Turk T. (2024) A rare case of cerebellar abscess caused by Nocardia cyriacigeorgica. SNI Digital. 15(413):1-4.

