David G Morrison*
Attending Physician, the Oncology Institute 11480 Brookshire Suite 309 Downey, CA 90241
*Corresponding author: David G Morrison, Attending Physician, The Oncology Institute 11480 Brookshire Suite 309 Downey, CA 90241.
Citation: Morrison DG. (2023) Partial Pituitary Failure Causing Profound Regression of Prostate Cancer Prior to Surgery: Case Report and Literature Review. J Can Ther Res. 3(1):1-4.
Received: April 3, 2023 | Published: April 23, 2023
Copyright© 2023 genesis pub by Morrison DG. CC BY NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JCTR.2023.3(1)-25
Abstract
54-year-old Cushingoid male with newly diagnosed prostate cancer was seen in consultation. He had very poor glucose control despite multiple medications for his diabetes and adherence to his diabetic diet. He had been noted to develop Cushingoid features for about 2 years prior to consultation. His prostate cancer gave rise to an enlarged prostate with a very hard nodule on palpation. The initial symptoms of his cancer were hematuria, pain and outlet obstruction. It was staged as T2cN0MO, Gleason 4+4 and PSA of 8.0 prior to any treatment. Half of the core biopsies were positive for prostate cancer with 10% or more of the cores having prostate cancer. When seen in consultation his PSA was less than one and his testosterone level was below 3 ng/dl. His hemoglobin A1c had fallen from 10.6 to 6.0 without any change in medications or diet. Further testing revealed essentially undetectable levels of ACTH and cortisol. At surgery only a tiny focus of prostate cancer,
<5mm, was found on one section of a normal sized, smooth bordered prostate specimen.
Introduction
Neoadjuvant ADT before radical prostatectomy, RP, is an area of active investigation. Multiple studies have noted an improvement in obtaining negative surgical margins, but no clear survival benefit has been reported. Near complete remission of disease has been seen and in one study the duration on ADT before surgery was noted to improve near complete remission status. Combinations of LHRH agonist with abiraterone and prednisone with or without enzalutamide have shown benefit as well. Multiple trials are ongoing [1]. An experiment of nature occurred and is presented here as a comment on neoadjuvant endocrine manipulation prior to RP.
Materials and Methods
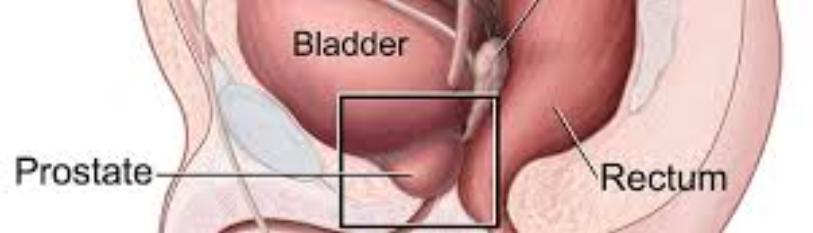
The patient was first seen for evaluation of hematuria, pain and nocturia 7 months prior to Medical Oncology consultation. Biopsy proof of adenocarcinoma of the prostate was obtained. Imaging showed an enlarged nodular prostate compressing the base of his bladder but no adenopathy. He had noncastrate levels of testosterone, a PSA of 8.0 ng/ml and a hemoglobin A1c of 10.6 % of total hemoglobin. He had Cushinghoid features noted over a year and one half prior to his diagnosis. He did not receive any hormonal manipulation prior to Medical Oncology consultation. At the time of that consultation his symptoms had completely resolved, testosterone levels were undetectable, and his PSA was less than 0.04 ng/ml. His hemoglobin A1c fell to 6.0 % of total hemoglobin. Due to concerns for pituitary failure additional labs and MRI of the pituitary were obtained. His ACTH and cortisol levels were undetectable. He had normal TSH and free T4 levels. His MRI was read as normal. He was started on replacement dosages of prednisone. His surgeon and anesthesiologist as well as his Primary Care physician were alerted to his partial pituitary failure. He underwent robotic prostatectomy without adverse incident. His Cushinghoid features are resolving, and he no longer requires medication for diabetes.
Results and Discussion
This patient’s near complete remission after pituitary apoplexy is as good or better than any response published (1, vide infra). The role of supraphysiologic then complete cortisol deficiency in this patient's response to castrate levels of testosterone is not known. His severe Cushinghoid features, and hyperglycemia suggest significant changes in multiple tissues. It is quite possible microenvironment changes from changes in cortisol plays a role in his excellent response. Pituitary apoplexy can be a silent event like in this patient and this event does not always cause complete pituitary failure [2]. Cortisol deficiency and loss of growth hormone are the two hormonal items adversely affected [2,3]. Neoadjuvant ADT has beneficial effects prior to radical prostatectomy but most patients do not demonstrate any effect.
Poppel et al [4] reported neoadjuvant ADT before RP decreased positive surgical margins in patients with T2 but not T3 prostate cancer. Abbas et al [5] reported a nonrandomized data set on neoadjuvant ADT reduced the mean PSA by>95%. Positive surgical margins dropped from 40.8% to 22.5%. Survival data showed no difference at 17.6 months. Similar results were reported by McClintock et al [6] using the National Cancer Database (2004—2014) noted a reduced hazard rate for positive surgical margins in patients with low to intermediate –risk. Soloway et al [7] in the initial Lupron Depot Neoadjuvant Study
Group that 3 months of ADT also reduced positive surgical margins but biochemical recurrence was only 3% better in the neoadjuvant group at 5 years. Aus et al [8] reported very similar results to those of Soloway with only a 2% reduction in biochemical recurrence in the neoadjuvant group. In a retrospective study of higher risk patients neoadjuvant ADT reduced biochemical relapse most in the group that had adjuvant radiation [9]. Shelley et al [10] in a systematic review and meta-analysis also noted neoadjuvant treatment improved positive margin, organ confinement and lymph node invasion rates. Meyer et al [11] reported the duration of neoadjuvant ADT (<92 vs >92 days) was a significant factor in reducing biochemical recurrence at both 4 and 8 years of follow-up. McKay et al [12] used intense ADT for 6 months prior to RP in high-risk patients.
Residual disease less than or equal to 5mm was seen in 22% of those patients in the most intensely treated patients, leuprolide, abiraterone, prednisone and enzalutamide. A recent review of neoadjuvant ADT summarizes the preceding and highlights the multitude of novel ongoing clinical trials. Again, neoadjuvant ADT most clearly improved pathologic down staging, decreased risk of positive surgical margins, decreased extracapsular extension and reduced seminal vesicle involvement. However, clear cut improvement in oncologic outcomes is lacking [1]. Some additional factors need to be coinhibited to improve responses to neoadjuvant ADT.
Conclusions
This experiment of nature argues for longer duration of neoadjuvant ADT. Perhaps LHRH antagonists might allow shorter durations of ADT to work as well as longer durations simply because significant suppression of testosterone levels occurs earlier with antagonists such as degarelix [13]. Rapid suppression of testosterone might not allow some prostate cancer clones to survive due to loss of paracrine factors or not allowing time for adaptation to a change in the microenvironment. Rapid declines in testosterone are seen with LHRH antagonists and pituitary apoplexy. There is evidence for cross talk between glucocorticoids and the androgen receptor [14]. Perhaps targeting the androgen receptor with enzalutamide, apalutamide or darolutamide along with ADT could produce a higher CR rate with subsequent improved overall survival. Alternatively, inhibition of glucocorticoids along with ADT might be a superior method to produce CR and prolong patient survival. Data indicates a cortisol effect on PSA levels in patients with significant life event stressors [15]. This reported experiment of nature could support either or both suppositions. These suppositions lend themselves to further laboratory and clinical experiments.
References
1. Perera M, Beech B, Escano MDJ, Gmelich C, Yip W, et al. (2022) Neoadjuvant systemic therapy prior to radical prostatectomy for clinically localized high-risk prostate cancer. Front Urol. 2.
2. Sinnadurai M, Cherukuri R, Moses R, Moses RG. (2010) Delayed pituitary apoplexy in a patient with prostate cancer treated with adjuvant gonadotropin releasing hormone agonist. J Clin Neurosci. 17(9):1201-3.
3. Valle MMD, Jesus OD. (2023) Pituitary apoplexy.PMID32644648
4. Poppel Herbrouck P. (1995) Neoadjuvant hormonal therapy before radical prostatectomy decreases the number of positive surgical margins in stage T2b prostate cancer: Interim results of a prospective randomized trial . J Urol. 1549(2 pt 1):429-34.
5. Abbas F, Kaplan M, Soloway MS. (1996) Induction androgen deprivation therapy before radical prostatectomy for prostate cancer—initial results. Br J Urol. 77(3):423-8.
6. McClintock TR, Landenberg NV , Cole AP, Lipsitz SR, Gild P, et al. (2019) Neoadjuvant androgen deprivation therapy prior to radical prostatectomy: Recent trends in utilization and association with postoperative surgical margin status. 26(1);297-05.
7. Soloway MS, Pareek K, Sharifi R, Wajsman Z, McLeod D, et al. (2002) Neoadjuvant androgen ablation before radical prostatectomy in cT2bNXM0 prostate cancer: 5-YEAR RESULTS. J Urol. 167(1):112-6.
8. Aus G, Abrahamsson PA, Ahlgren G, Hugosson J, Lundberg S, et al. (2002) Three-month neoadjuvant hormonal therapy before radical prostatectomy: A 7 –year follow-up of a randomized controlled trial. BJU Int. 90(6):561-66.
9. Tosco L, Laenen A, Briganti A, Gontero P, Karnes RJ, et al. (2017) The survival impact of neoadjuvant hormonal therapy before radical prostatectomy for treatment of high-risk prostate cancer. Prostate Cancer Prostatic Dis. 20(4):407-12.
10. Shelley MD, Kumar S, Wilt T, Staffurth J, Coles B, et al. (2009) A systematic review and meta- analysis of randomized trials of neoadjuvant hormone therapy for localized and locally advanced prostate carcinoma. Cancer Treat Rev. 35(1):9-17.
11. Meyer F, Bairati I, Bedard C, Lacombe L, Tetu B, et al. (2001) Duration of neoadjuvant androgen deprivation therapy before radical prostatectomy and disease-free survival in men with prostate cancer. Urology. 58(2 suppl 1): 71-7.
12. McKay RR, Xie W, Ye H, Fennessy FM, Zhang Z, et al. (2021) Results of a randomized phase II trial of intense androgen deprivation therapy prior to radical prostatectomy in men with high-risk localized prostate cancer. J Urol. 206(1):80-87.
13. https://firmagon.com/
14. Fernandino JL, Hattori RS, Kishii A, Strussmann CA, Somoza GM, et al. (2012) The cortisol and androgen pathways cross talk in high temperature induced masculinization: The 11 beta- hydroxysteroid dehydrogenase as a key enzyme. Endocrinology. 153(12):6003-11.
15. Gidron, Y, Fabre, B, Grosman, H et al Life events, cortisol and levels of prostate specific antigen: A story of synergism doi.org/10.1016/j.psyneuen.2010.11.01.