Novel Method of Using Proximal Femoral Triangle and Intermediate Femoral Cutaneous Nerve Blocks to Reduce Procedural Pain for Knee Genicular Radiofrequency Ablation
Manish Mittal1* and Yunis Fazaldin2
1Consultant in Anaesthesia and Chronic Pain, George Eliot hospital, UK MBBS, FRCA, FFPMRCA, EDRA, EDAIC
2MBBS BSc George Eliot Hospital NHS Trust
Abstract
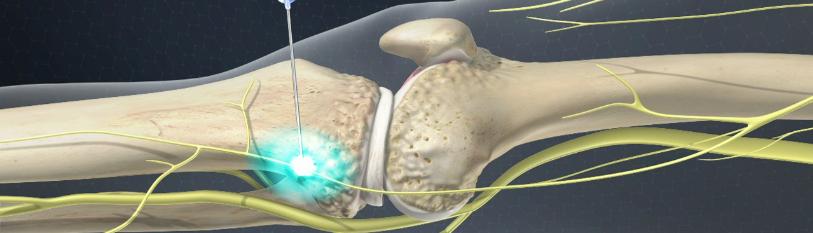
Recent dermatomal mapping of the anterior cutaneous branches of the femoral nerve by Siska Bjørn and colleagues has created extreme enthusiasm about its potential use for various clinical indications [1]. Application of regional anesthesia in chronic pain and vice versa is becoming more common and this article describes a similar application. The conventional knee genicular nerve radiofrequency ablation (RFA) and cooled RFA is commonly performed for chronic knee pain and can be very painful, requiring sedation and supplement analgesia. This article highlights the first case on the usefulness of the saphenous and anterior femoral cutaneous nerve and nerve to vastus medialis blocks (Intermediate femoral cutaneous nerve and proximal femoral triangle block) for procedural pain in knee genicular RFA.
Keywords
Medial femoral cutaneous nerve (MFCN); Intermediate femoral cutaneous nerve (IFCN); Proximal femoral triangle (PFT); Superficial femoral artery (SFA); Radiofrequency ablation (RFA); Numerical rating scale (NRS).
Background and Objectives
Anatomy [1,2]: The anterior division of the femoral nerve has two cutaneous branches: the medial femoral cutaneous nerve (MFCN) and the intermediate femoral cutaneous nerve (IFCN). MFCN is proximally lateral to the superficial femoral artery as it passes near to the medial border of sartorius. It crosses the artery anteriorly and reaches the medial side where it branches to anterior and posterior branches. Before doing so, it sends a few rami through the fascia lata to supply the skin of the medial side of the thigh, near the long saphenous vein. Branching into anterior and posterior can be variable and can occur before the nerve crosses the femoral artery.
Introduction
The Medial femoral cutaneous nerve - anterior branch (MFCN-A)
Descends alongside the sartorius and perforates the fascia lata beyond the mid-thigh. It then divides into a branch that supplies the skin as distal as the medial aspect of the knee, and another that runs lateral and connects with the infrapatellar branch of the saphenous nerve. Recent cadaveric studies shows that it also innervates deeper structures including medial retinaculum [3].
The medial femoral cutaneous nerve - posterior branch (MCFN-P)
Descends along the posterior border of sartorius to the knee, pierces the fascia lata, and connects with the saphenous nerve and gives off several cutaneous rami, some as far as the medial side of the leg. The nerve contributes to the sub-sartorial plexus.
The intermediate femoral cutaneous nerve (IFCN)
Usually pierces the fascia lata ~8 cm below the inguinal ligament, either as two branches or as one trunk that quickly divides into two. These descend down the anterior aspect of the thigh, supplying the skin as far as the knee and ending in the peri-patellar plexus. The lateral branch of the IFCN communicates with the femoral branch of the genitofemoral nerve, frequently piercing sartorius and sometimes supplying it.
Recent brilliant work by Siska Bjørn and colleagues highlighted the importance of proximal femoral triangle block (FTB) in anaesthetizing both MFCN and IFCN, which are sometimes spared in adductor canal block, also the importance of MFCN in analgesia (superficial and deep) of anterior knee [4].
For procedural purposes the author suggests using both proximal FTB and IFCN block in the fat filled tunnel superficial to sartorius muscle (SAM) for adequate analgesia and improved procedural pain.
Method
Inspired by the work by Bjørn and colleagues, the author used both proximal FTB and IFCN blocks in knee genicular RFA. We present two case reports 8 weeks apart on patients requiring conventional genicular nerve blocks (superomedial, inferomedial, and superolateral).
Case Report 1
A 44-year-old male with right knee pain and moderate osteoarthritis was referred to the pain clinic as he was not appropriate for a total knee replacement. His pain was mainly in the medial compartment of his right knee. He had a successful diagnostic knee genicular nerve RFA. This was performed using local anaesthetic, steroid, and 20mg depomedrone, with more than 60% pain relief.
He was consented for the procedure and the study on attendance. It was explained that the nerve blocks are the application of an already established pain procedure from regional anesthesia, and not an entirely new technique.
Ultrasound guidance was used to locate the proximal femoral triangle, which was found on the lateral side of the femoral artery, close to the medial border of the sartorius. The IFCN was found on the anterior surface of the sartorius. 15mL of 0.25% Levo-bupivacaine was used to block the nerves at both locations. Skin analgesia was confirmed using both light and sharp touch.
The RFA consisted of two lesions being made at each level. During the procedure, there was no pain except during the 90 seconds when the RFA temperature reached 80°C. This was rated as 3-4/10 on NRS (numerical rating score) and was described as a pressure within the knee.
Case Report 2
A 65-year-old female with bilateral knee pain and moderate arthritis was referred to the pain clinic as she was not suitable for total knee replacement. Her pain was predominantly in the medial compartments. MRI imaging revealed a reduction in the medial and patellofemoral joint spaces, with associated degenerative changes. Bilateral diagnostic knee genicular blocks were successfully performed with local anaesthetic, steroid, and 20mg depomedrone, with more than 50% pain relief.
Proximal FTB and IFCN block was performed as described before. Local anaesthetic (LA) of the skin was performed on the first injection only. Unilateral RFA was completed successfully. The patient described the procedural pain as a lot of pressure only during RFA, with an NRS of 3-4/10. Subsequent pain diary analysis showed an overall knee pain score reduction from 8 to 3 when followed up in one month.
Both patients described minimal procedural pain throughout the RFA, which was mainly pressure sensation.
Ultrasound guided proximal FTB and IFCN block: procedure
Step 1: Scan at the femoral crease and locate the femoral artery.
Step 2: Scan the femoral artery distally until it reaches the medial border of the sartorius. At this point the MFCN lies lateral to the femoral artery, as well as the saphenous nerve and the nerve to vastus medialis. These landmarks form the proximal femoral triangle [4]. IFCN lies on the anterior surface of the sartorius in the fat filled tunnel between the fascia lata and the muscle.
Step 3: Continue scanning inferiorly until the MFCN crosses over and becomes medial to the femoral artery. This is followed by anterior division (MFCN-A) moving over the sartorius, and posterior division (MFCN-P) lying between Femoral Artery (FA), Adductor Longus (AL) and Facia Lata (FL) [1].
The Proximal femoral triangle block with intermediate femoral triangle block is suggested at step 2.
MFCN-A block can be blocked separately at the lower border of sartorius.
Lateral Medial
Figure 1: USG image of proximal femoral triangle with Sartorius, IFCN and SFA (Superficial femoral artery).
Lateral Medial
Figure 2: USG image of proximal femoral triangle with Sartorius, MFCN and SFA (Superficial femoral artery).
Results
This is the first case report documenting the use of a proximal femoral triangle and intermediate femoral cutaneous nerve block for knee genicular nerve group radiofrequency ablation. This technique has not yet been described in patients who have provided procedural pain data. Our findings suggest that this approach improved procedural pain during knee genicular nerve RFA.
Further research
Medial femoral cutaneous nerve anterior branch block has shown to be promising in anterior knee pain after knee surgery (replacement) and Chronic pain procedures involving knee (knee genicular RFA), isolated MFCN-A can also be of benefit in RFA of genicular nerves. Further studies with larger patient group are needed to delineate its use in such procedures.
Video links
Link 1: https://youtu.be/-2ieUrl8JjI (IFCN and MFCN with Proximal femoral triangle)
Link 2: https://youtu.be/gif6RYLFuuM (MFCN and Proximal femoral triangle)

