Mohammad Azizur Rahman1*, Umme Habiba2
1Department of Biochemistry and Molecular Biology, Jahangirnagar University, Dhaka, Bangladesh
2Incepta Pharmaceuticals Limited, Dhaka, Bangladesh
*Corresponding author: Mohammad Azizur Rahman, Department of Biochemistry and Molecular Biology, Jahangirnagar University, Dhaka, Bangladesh.
Citation: Rahman MA, Habiba U. (2023) Neurobiochemical Cross-Talk Between Dengue Virus and the Nervous system. J Neuro Sci Res. 3(2):1-6.
Received: December 5, 2023 | Published: December 21, 2023
Copyright ©️2023 genesis pub by Rahman MA, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Dengue, a severe and fatal viral disease, has become a global crisis. The notorious causative agent of dengue is the dengue virus (DENV). Though multi-organ manifestations of the dengue fever have been documented, less report has been publicized regarding the neuro-biochemical manifestations of DENV. This paper illustrates the neuro-biochemical, neuro-pathological and associated features with a view to aid in formulating the increasing dengue affected global populace.
Keywords
Arbovirus; Immunoglobulin; Central nervous system; Peripheral nervous system; Serotype
Introduction
Dengue, the most common arboviral disease, has been taking a heavy toll globally [1]. Dengue is caused by the dengue virus (DENV) that is a single-stranded RNA virus and belongs to the family Flaviviridae [2]. Five serotypes of DENV (DENV-1, -2, -3, -4, -5) have been reported to be the culprit of this fastest spreading tropical disease and the second-most acute febrile disease of the travelers worldwide [3]. Though neurological involvement of dengue virus had been noticed since 1976, less attention had been paid towards amelioration of dengue-induced neurobiochemical alteration [4]. As currently, dengue has been plaguing different nations of the world severely, time is up to delve into the neuronal involvement and remedy of the dengue virus infection [5]. In 2009, the world health organization (WHO) classified dengue into three types: dengue with no signs, dengue with signs and severe dengue [6].
Narcoviolence of the Dengue Virus
Denv is neurovirulent. Neurovirulence of this virus in the central nervous system (CNS) had been ascertained through presence of viral RNAs, proteins and host immunoglobulins generated against this virus [7]. DENV-2 and DENV-3 serotypes had been found to be most neurovirulent [8]. Presence of DENV in the cerebrospinal fluid (CSF) has confirmed this viruse’s neuropathological involvement [9]. DENV had been reported to disrupt the blood brain barrier of the experimental animals [10]. Autoimmune reaction leading towards immunoreactivity of the neurons and altered metabolic fates in the hemorrhagic dengue fever had been observed [11].
Denv entry into the CNS
Hematogenous route has been considered to be the most direct entrance of the DENV to the CNS [12]. Normally, the blood brain barrier (BBB) prevents the entry of external components into the CNS. During DENV infection, the BBB might have been compromised anyway or the BBB might have undergone any alteration allowing the safe entry of the DENV as well as favoring the consequent neuro-inflammatory processes [13]. Dysregulation of the endothelial cell (EC) homeostasis directly by the DENV or DENV secreted components or pro-inflammatory mediators of DENV-infected cells could aid in ravaging the cascade [14]. Binding of the DENV to the EC activates the rho-associated coiled coil kinase (ROCK) as well as vimentin alteration that facilitates viral replication and assemblage of virion particles [15]. EC membrane sugars especially heparin sulfate acts as viral attractant. More advertantly, heat shock protein (HSP 70, HSP 90), CD 14, CD 60, ICAM 30, laminin act as EC receptor to the DENV [16]. Entrance of the DENV to the nervous system creates a “cytokine storm” that ultimately leads towards neuro-biochemical alteration leading towards physiological and psychological abnormalities of the dengue patient [17].
CNS Complications
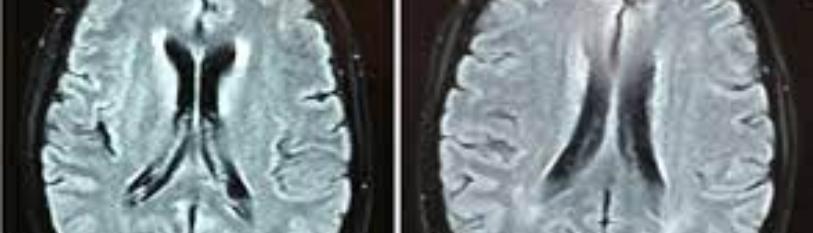
Encephalitis
Encephalitis has been found common with all the three dengue types [18].
Encephalopathies
Dengue virus induced encephalopathy had been manifested through behavioral alteration, cognitive impairment, anxiety, depression, aggression, mania and personality change [19]. About 50% of the dengue patients have been linked with encephalopathy and emotional alteration [20]. Dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS) correlate with anoxia, brain edema, hemorrhage, hyponatremia, renal or hepatic abnormalities [21]. Mutation of the envelope glycoprotein (replacement of alanine by valine at position 173) of DENV-2 had been implicated in encephalopathy [22]. Electroencephalograph (EEG) of the encephalopathics show epilepsia partialis continua, seizures and burst suppression [23].
Seizures
Seizures alone or associated with encephalopathy and encephalitis have frequently been observed in dengue patients [24]. Children have been found much prone to seizures than the adults [25].
Meningitis
Dengue associated meningitis, though previously less encountered, has become a commonplace nowadays [26]. Menigitis along with headache, neck rigidity, decreased platelet count are the common manifestations [27].
Stroke
Hemorrhagic and ischemic strokes have been linked with DENV infection [28]. These may be due to increased permeability of blood vessels and leakage of plasma [29]. These type of dengue patients suffer from speech difficulty and paralysis [30]. Other cerebellar syndromes include nystagmus and gait abnormalities [31]. Hypokalemic paralysis of the dengue patients has been linked with increased catecholamine mediated increased urinary excretion of potassium and renal tubular acidosis [32]. Neuro-muscular consequence such as transient muscular dysfunction has also been manifested in dengue patients [33]. Elevated levels of creatinine phosphokinase (CPK) have been found in the serum of dengue patients suffering from neuro-muscular dysfunction [34].
PNS Complication
Guillain-Barré Syndrome
Guillain–Barré syndrome (GBS) is a peripheral polyneuropathy that causes paralysis through blockade of motor neurotransmission [35]. Among dengue patients, the children usually fall a victim to GBS [36]. Though the exact mechanism is yet to unveil, immunocytes and pro-inflammatory mediators such as tumor necrosis factors (TNF), interleukins (ILs) and cytokines might be involved in DENV induced GBS pathogenesis [37].
Neuritis
Neuritis associated with dengue involve abducens, phrenic and thoracic nerve palsy, peripheral facial palsy and brachial neuritis [38]. Cranial nerve palsy, retinal vasculopathy and optic neuropathy are some neuro-ophthalmic complications of DENV infection [39].
Denv Induced Parkinsonism
DENV-induced parkinsonism could be considered as a novel manifestation of this catastrophe [40]. Though the exact mechanism could not be outlined yet, disturbed neurotransmission and altered production and management of the neurotransmitters could lay the foundation of viral parkinsonism in dengue patients.
Conclusion
Dengue has been creating global havoc. Neuro-biochemical manifestations of dengue and dengue virus (DENV) has attracted less attention. Time is up for considering the neuro-biochemical underpinnings of dengue and DENV and chalking out appropriate measures for the betterment of global public health. Thus, the government and non-government organizations, policy makers, health professionals, care givers, donor agencies and research and development organizations should formulate necessary strategies to save the global populace from dengue and DENV-mediated patho-physiological and neuro-biochemical hallmarks.
Acknowledgement
Authors gratefully thank Jahangirnagar University and the University Grants Commission (UGC) of Bangladesh for providing all the supports.
References
1. Guzman MG, Halstead SB, Artsob H, Buchy P, Farrar J, et al. (2010) Dengue: A continuing global threat. Nat Rev Microbiol. 8(12supply):S7-16.
2. Brady OJ, Gething PW, Bhatt S, Messina JP, Brownstein JS, et al. (2012) Refining the global spatial limits of dengue virus transmission by evidence-based consensus. PLoS Negl Trop Dis. 6(8):e1760.
3. World Health Organization. (2021) Dengue and severe dengue. World Health Organization, Geneva, Switzerland.
4. World Health Organization. (2011) Comprehensive guidelines for prevention and control of dengue and dengue haemorrhagic fever. Revised and expanded edition. World Health Organization, Geneva, Switzerland.
5. Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, et al. (2013) The global distribution and burden of dengue. Nature. 496(7446):504-07.
6. Monath TP. (1994) Yellow fever and dengue - the interactions of virus, vector and host in the re-emergence of epidemic disease. Seminars in virology. 5:133-45.
7. Halstead SB. (1998) Emergence mechanisms in yellow fever and dengue. Emerging Infections. 2:65-79.
8. Murthy JM. (2010) Neurological complications of dengue infection. Neurol India. 22(8):581-84.
9. Huy NT, Van Giang T, Thuy DHD, Kikuchi M, Hien TT, et al. (2013) Factors associated with dengue shock syndrome: A systematic review and meta-analysis. Plos Negl Trop Dis. 7(9):e2412.
10. Carabali M, Hernandez LM, Arauz MJ, Villar LA, Ridde V. (2015) Why are people with dengue dying? A scoping review of determinants for dengue mortality. BMC Infect Dis. 15:301
11. Kadam DB, Salvi S, Chandanwale A. (2016) Expanded Dengue. J Assoc Physicians India. 64(4):59-63.
12. Gera C, George U. (2010) Acute disseminating encephalomyelitis with hemorrhage following dengue. Neurol India. 58(4):595-6.
13. Malheiros SM, Oliveira AS, Schmidt B, Lima JG, Gabbai AA. (1993) Dengue. Muscle biopsy findings in 15 patients. Arq Neuropsiquiatr. 51(2):159-64.
14. Kalita J, Misra UK, Mahadevan A, Shankar SK. (2005) Acute pure motor quadriplegia: Is it dengue myositis? Electromyogr Clin Neurophysiol. 45(6):357-61.
15. Misra UK, Kalita J, Syam UK, Dhole TN (2006) Neurological manifestations of dengue virus infection. J Neurol Sci. 244(1-2):117-22.
16. Solbrig MV, Perng GC. (2015) Current neurological observations and complications of dengue virus infection. Curr Neurol Neurosci Rep. 15(16):29.
17. Kyaw AK, Ngwe Tun MM, Nabeshima T, Buerano CC, Ando T, et al. (2019) Japanese Encephalitis- and Dengue-Associated Acute Encephalitis Syndrome Cases in Myanmar. Am J Trop Med Hyg. 100(3):643-46.
18. Mello CDS, Cabral-Castro MJ, Silva de Faria LC, Peralta JM, Puccioni-Sohler M. (2020) Dengue and chikungunya infection in neurologic disorders from endemic areas in Brazil. Neurol Clin Pract. 10(6):497-502.
19. Cunha MDP, Duarte-Neto AN, Pour SZ, Hajjar LA, Frassetto FP, et al. (2021) Systemic dengue infection associated with a new dengue virus type 2 introduction in Brazil - a case report. BMC Infect Dis. 21(1):311.
20. Miagostovich MP, dos Santos FB, Fumian TM, Guimarães FR, da Costa EV, et al. (2006) Complete genetic characterization of a Brazilian dengue virus type 3 strain isolated from a fatal outcome. Mem Inst Oswaldo Cruz. 101(3):307-13.
21. Seet RC, Lim EC. (2007) Dysarthria-clumsy hand syndrome associated with dengue type-2 infection. J Neurol. 254(8):1129-30.
22. Vargas-Sánchez A, Chiquete E, Gutiérrez-Plascencia P, Castaneda-Moreno V, Alfaro-Castellanos D, et al. (2014) Cerebellar hemorrhage in a patient during the convalescent phase of dengue fever. J Stroke. 16(3):202-04.
23. Ngwe Tun MM, Muthugala R, Nabeshima T, Soe AM, Dumre SP, et al. (2020) Complete genome analysis and characterization of neurotropic dengue virus 2 cosmopolitan genotype isolated from the cerebrospinal fluid of encephalitis patients. PLoS One. 15(6):e0234508.
24. Sahu R, Verma R, Jain A, Garg RK, Singh MK, et al. (2014) Neurologic complications in dengue virus infection: a prospective cohort study. Neurology. 83(18):1601-09.
25. Puccioni-Sohler M, Orsini M, Soares CN. (2012) Dengue: A new challenge for neurology. Neurol Int. 4(3):e15.
26. Verma R, Sahu R, Holla V. (2014) Neurological manifestations of dengue infection: A review. J Neurol Sci. 346(1-2):26-34.
27. Matlani M, Chakravarti A, Rawal A, Kashyap B, Gurtoo A. (2009) Dengue encephalitis: An entity now common in dengue-prone regions. Tropical Doctor. 39(2):115-16.
28. Larik A, Chiong Y, Lee LC, Ng YS. (2012) Longitudinally extensive transverse myelitis associated with dengue fever. BMJ Case Rep. 2012:Bcr1220115378.
29. De Sousa AM, Alvarenga MP, Alvarenga RM. (2014) A cluster of transverse myelitis following dengue virus infection in the brazilian Amazon region. Trop Med Health. 42(3):115-20.
30. Mo Z, Dong Y, Chen X, Yao H, Zhang B. (2016) A cute transverse myelitis and subacute thyroiditis associated with dengue viral infection: A case report and literature review. Exp Ther Med. 12(4):2331-5.
31. Mota MT, Estofolete CF, Zini N, Terzian AC, Gongora DV, et al. (2017) Transverse Myelitis as an Uunusual complication of dengue fever. Am J Trop Med Hyg. 96(2):380-1.
32. Yamamoto Y, Takasaki T, Yamada K, Kimura M, Washizaki K, et al. (2002) Acute disseminated encephalomyelitis following dengue fever. J Infect Chemother. 8(3):175-7.
33. Tenembaum S, Chitnis T, Ness J, Hahn JS. (2007) International pediatric MS study group. Acute disseminated encephalomyelitis. Neurology. 68(16 supply):S23-36
34. Weeratunga PN, Caldera HP, Gooneratne IK, Gamage R, Perera WS, Ranasinghe GV, et al. (2014) Spontaneously resolving cerebellar syndrome as a sequelae of dengue viral infection: A case series from Sri Lanka. Pract Neurol. 14(13):176-8.
35. Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. (2013) Neurological complications of dengue virus infection. Lancet Neurol. 12(9):906-19.
36. Li GH, Ning ZJ, Liu YM, Li XH. (2017) Neurological Manifestations of Dengue Infection. Front Cell Infect Microbiol. 7:449.
37. Basu A, Chaturvedi UC. (2008) Vascular endothelium: the battlefield of dengue viruses. FEMS Immunol Med Microbiol. 53(3):287-99.
38. Bastidas-Legarda LY, Beltrán EO, Camacho-Ortega SJ, Castellanos JE. (2019) Dengue virus infection of blood-brain barrier Cells: Consequences of severe disease. Front Microbiol. 10:1435.
39. Viswanathan S, Botross N, Rusli BN, Riad A. (2016) Acute disseminated encephalomyelitis complicating dengue infection with neuroimaging mimicking multiple sclerosis: A report of two cases. Mult Scler Relat Disord. 10:112-5.
40. Salazar MI, Pérez-García M, Terreros-Tinoco M, Castro-Mussot ME, Diegopérez-Ramírez J, et al. (2013) Dengue virus type 2: Protein binding and active replication in human central nervous system cells. Scientific World Journal. 2013:904067.
41. Lin C-F, Chiu S-C, Hsiao Y-L, Wan S-W, Lei H-Y, et al. (2005) Expression of cytokine, chemokine, and adhesion molecules during endothelial cell activation induced by antibodies against dengue virus nonstructural protein 1. J Immunol. 174(1):395-403.