Near Complete Giant Intracranial Aneurysm Mimicking Anaplastic Glioma: A Rare Case Report and Surgical Management
Bikash Bhandari1*, Sai Charan Sharma1, Sushmita Pandey1, Sandesh Dhakal1 and Diwas Bhandaris
1MBBS, College of Medical Sciences
2MBBS, Lumbini Medical College
*Corresponding author: Bikash Bhandari, MBBS, College of Medical Sciences.
Citation: Bhandari B, Sharma SC, Pandey S, Dhakal S, Bhandari D. Near Complete Giant Intracranial Aneurysm Mimicking Anaplastic Glioma: A Rare Case Report and Surgical Management. J Neurol Sci Res. 4(1):1-6.
Received: June 25, 2024 | Published: July 12, 2024
Copyright©️ 2024 genesis pub by Bhandari B, et al.CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non-Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Introduction
A large spherical intracranial mass can sometimes be misdiagnosed due to the lack of typical radiographic features. Though rare, Giant intracranial aneurysm with thrombosis (GIAs) must be considered in differential diagnoses to ensure the optimal surgical approach and resection of the lesion.
Materials and Method
We present a case of a 34-year-old female patient who complained of gradual onset and progressive weakness of the right side of her body for 5 days, along with multiple episodes of vomiting, dizziness, slurring of speech, and being unable to speak. An MRI of the brain was conducted, and a time-resolved angiography with interleaved stochastic trajectories (TWIST-MRI) was utilized to assess the vascular origin of the lesion.
Results and Discussion
The MRI revealed a near-completely thrombosed left internal carotid aneurysm with surrounding edema and a mass effect with midline shift. Initially, the lesion was considered a glioma due to its atypical radiographic features. However, TWIST-MRI indicated the vascular origin of the lesion.. If typical radiographic features are absent, completely thrombosed GIAs with parent vessel thrombosis, being rare lesions, might be misdiagnosed. Thus, in the case of an intracranial spherical mass with signs of intralesional hemorrhage and mural calcifications, the presence of a completely thrombosed GIA should be considered as a possible differential diagnosis.
Keywords
Giant intracranial aneurysm; Intraluminal thrombosis; Clipping; Parent vessel; Anaplastic glioma
Introduction
Giant intracranial aneurysms (GIAs) are rare and heterogeneous lesions with complex vascular anatomy [1] and represent almost 5% of intracranial aneurysms (IAs) [2]. These aneurysms typically present symptoms between the 4th and 7th decades of life, with a female to male ratio of 1:1 to 3:1 [2], and intraluminal thrombosis occur in 10 to 30 % of cases [3]. However, a complete aneurysmal thrombosis is extremely rare [4]. The majority of these aneurysms are located in the internal carotid artery (ICA) and in the middle cerebral artery (MCA), with the anterior cerebral artery (ACA) being an exceptional location [1].
In this report, we present an unusual case of a completely thrombosed GIA of the left ACA that was initially misdiagnosed as glioma because of the lack of typical radiographic features.
Case Presentation
A 34-year-old female with no comorbidities and no drug history presented with intermittent weakness of the right side of the body for 15 days with multiple vomiting episodes during the last 3 days, along with a progressive Holocephali headache and slurring of speech with a tingling sensation in the right hand. Ptosis and loss of the nasolabial fold of the right side were also present. Hyperreflexia of the knee and ankle jerk along with hypoesthesia on the right side of the body, predominantly on the lower limb, with intact reflexes and sensation on the left side, along with intact bowel and bladder control. The left pupil was dilated symmetrically and showed no reaction to light or near objects. The right pupil was intact with a normal response to light and near objects. MRI and MRA findings of a near-completely thrombosed left ICA giant aneurysm (likely cavernous part) with surrounding edema and mass effect with midline shift. There was no fever, no weight loss, and no loss of consciousness. The rest of the physical examination showed an ataxic gait. During the hospital stay, the patient developed a focal seizure, starting as a tingling sensation in the right hand, which generalized to a tonic clinic seizure, and was treated with sodium valproate.
Radiological Finding
Figure 1
Figure 2
Figure 3
Figure 4
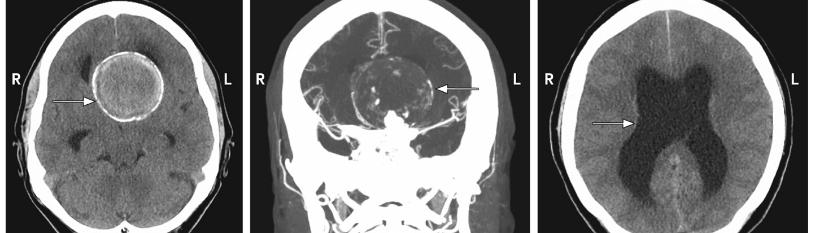
Figure 1-4: MRI findings of a large, well-defined, near-completely thrombosed left ICA aneurysm (mostly likely cavernous part) measuring ~6.09 x 5.94 x 6.17cm with laminated and heterogeneous internal contents of various stages of blood products. The neck of the aneurysm is not visualized. The lesion appears isotomically hyperintense on TIW and predominantly hypointense on T2W and FLAIR images. DWI shows no restriction of the lesion. A post-contrast study shows peripheral enhancement of the aneurysm. Surrounding the lesion, there is moderate edema. The lesion is extending to the left temporal lobe and the anteroinferior aspect of the left frontal lobe. The mass effect is noted as evident by a midline shift of ~10.2mm to the contralateral side with compression of the ipsilateral lateral ventricle and dilatation of the contralateral lateral ventricle (subfalcine herniation). The left basal ganglia and thalamus are compressed by the lesion. Postero-inferiorly, the lesion is compressing the midbrain. The lesion is compressing the left posterior cerebral artery with a displacement of the basilar.
Laboratory Findings
Blood and cerebrospinal fluid (CSF) screenings showed no signs of infection. No tumor cells were found in the CSF.Parasitological examination for Toxoplasmosis, Echinococcus, and neurocysticercosis. Tumor markers for astrocytoma, gliomas, schwannoma, and lymphoma were negative, along with negative serological testing for HIV in both blood and CSF.
Surgical Treatment
A left temporoparietal craniotomy was performed. The preparation showed a very hard cystic lesion, evoking the differential diagnosis of a thrombosed aneurysm. The aneurysmal parent vessel was found. The intraoperative Indocyanine green CT angiography demonstrated a very low blood flow in this thrombosed vessel. After clipping the parent vessel, the aneurysmal sac was opened meticulously, and the thrombi and calcifications were resected.
Postoperative course and follow-up
The patient recovered well postoperatively, with no neurological deficts. A DSA showed no aneurysmal remnants after clipping. Collateral circulation from both the MCAs and the posterior circulation was observed. At the 4-month follow-up, the patient recovered from the operation and could walk without assistance with increased muscle power, a complete recovery of facial palsy, and resolving dysarthria with a normal gag and cough reflex and seizure-free seizure from the first postoperative day.
Discussion
The natural history of GIAs is marked by three pathological events: spontaneous thrombosis, growth leading to a mass effect, and rupture causing a subarachnoid hemorrhage [2]. These are characterized by a high mortality rate, essentially for aneurysms located on the posterior circulation [5], as the rupture rate in 5 years ranges between 40 and 50% [6]. Most often, including in our case, GIAs are diagnosed during a pseudo tumoral syndrome, where the mass effect of the aneurysm causes a gradual onset of symptoms neurologic deterioration [7].
Complete intraluminal thrombosis is uncommon and occurs, especially in large and giant cerebral aneurysms, in 13–20% of cases [4]. This phenomenon is attributed to endothelial damage caused by hemodynamic stress On the aneurysmal wall [4].
CT angiogram findings Non-visualization of the left internal carotid artery (CI-C7 segments). The distal portion of the C7 segment is opacified. The left MCA is poorly opacified. The A1 segment of the left anterior cerebral artery is also not visualized. At the cavernous segment of the left ICA, there is a large, well-defined heterogeneous lesion measuring ~6.09 x 5.94 x 6.17 em with peripheral calcification. It is displacing the left anterior cerebral artery superolateral. Moderate surrounding edema with mass effect causing midline shift to the contralateral side, compression of the left basal gangial and thalamus, and compression of the left PCA by the rest of the bilateral ACA, right MCA, PCA normal in course, caliber, and outline.
MRI findings of a large, well-defined, near-completely thrombosed left ICA aneurysm (mostly likely cavernous part) measuring ~6.09 x 5.94 x 6.17cm have laminated and heterogeneous internal contents of various stages of blood products. The neck of the aneurysm is not visualized. The lesion appears isotomically hyperintense on TIW and predominantly hypointense on T2W and FLAIR images. DWI shows no restriction of the lesion. There is a thin peripheral rim of calcification. A post-contrast study shows peripheral enhancement of the aneurysm. Surrounding the lesion, there is moderate edema. The lesion is extending to the left temporal lobe and the anteroinferior aspect of the left frontal lobe. The mass effect is noted as evident by a midline shift of ~10.2mm to the contralateral side with compression of the ipsilateral lateral ventricle and dilatation of the contralateral lateral ventricle (subfalcine herniation). The left basal ganglia and thalamus are compressed by the lesion. Postero-inferiorly, the lesion is compressing the midbrain. The lesion is compressing the left posterior cerebral artery with displacement of the basilar artery. The left MCA is also not visualized. However, the M3 segment is seen. The left optic nerve is buckled by the mass effect. No proptosis. Here is erosion with thinning of the left petrous apex and left temporal bone by the lesion. There is erosion of the sphenoid bone and also of the left greater wing of the sphenoid bone with its bowing anteriorly. Balloning of the sella with compression of the pituitary gland. The posterior pituitary bright spot is not visualized. Wall calcification of the bilateral vertebral artery and the right middle cerebral artery. MRA shows non-visualization of the left internal carotid artery distal to the carotid bifurcation (s/o thrombus).
The exact mechanism behind the spontaneous thrombosis of an aneurysm and its parent artery remains unknown. Theories suggest that local stretching, compression and distortion of the ICA, influenced by dural folds and bony structures in the cavernous segment, could explain this complication [10].
Conclusion
Near-complete thrombosis of giant intracerebral aneurysms with parent vessel thrombosis are rare lesions that might be misdiagnosed if typical radiographic features are missing. Thus, in the case of an intracranial spherical mass with signs of intralesional hemorrhage and mural calcifications, the presence of a completely thrombosed GIA should be considered as a possible differential diagnosis.
References
- Nurminen V, Lehecka M, Chakrabarty A, Kivisaari R, Lehto H, et al. (2014) Anatomy and morphology of giant aneurysms—an angiographic study of 125 consecutive cases. Acta Neurochir.156(1):1-10.
- Lonjon M, Pennes F, Sedat J, Bataille B. (2015) Epidemiology, genetic, natural history, and clinical presentation of giant cerebral aneurysms. Neurochirurgie. 61(6):361-65.
- dos Santos MLT, Spotti AR, dos Santos RMT, Borges MA, Ferrari AF, et al. (2013) Giant intracranial aneurysms: morphology and clinical presentation. Neurosurg Rev. 36(1):117–22.
- Das KK, Singh G, Pandey S, Bhaisora KS, Jaiswal A, et al. (2018) Completely thrombosed giant intracranial aneurysm with spontaneous thrombosis of the parent artery: is it nature's divine intervention and a self-cure? World Neurosurg. 118:132-38.
- Drake CG. (1979) Giant intracranial aneurysms: experience with surgical treatment in 174 patients. Clin Neurosurg. 26:12-95.
- Wiebers DO. (2003) Investigators ISoUIA Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362(9378):103-10.
- Choi IS, David C. (2003) Giant intracranial aneurysms: development, clinical presentation, and treatment. Eur J Radiol. 46(3):178-94.

