Myasthenia Gravis Crisis and Rescue in Late-Onset Myasthenia Gravis Precipitated by COVID-19 Infection
Corrado Angelini*
*Department Nerosciences University of Padova, Italy
*Corresponding author: Corrado Angelini, Department Nerosciences University of Padova, Italy
Citation: Angelini C. (2024) Myasthenia Gravis Crisis and Rescue in Late-Onset Myasthenia Gravis precipitated by COVID-19 infection. J Clin Pract Med Case Rep. 1(1):1-4.
Received: January 11, 2024 | Published: January 29, 2024
DOI: https://doi.org/10.52793/JCPMCR.2024.1(1)-04
Introduction
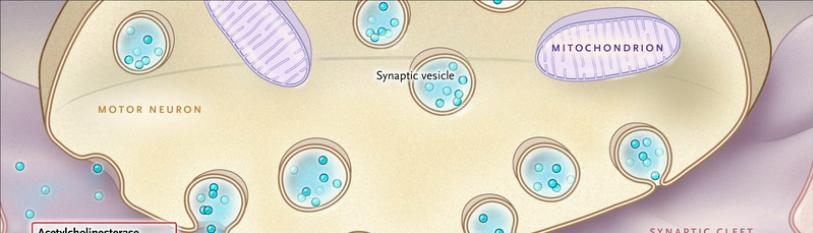
Myasthenia gravis (MG) is an autoimmune neuromuscular disorder characterized by ocular, skeletal, and respiratory muscle weakness. Antibodies that with complement attack the receptors responsible for muscle contraction at the neuromuscular junction. Late-onset myasthenia gravis refers to cases where the symptoms develop after the age of 50 and have increasingly been observed in older men recently.
The COVID-19 pandemic caused by the SARS-CoV-2 virus has raised concerns regarding its impact on individuals with pre-existing health conditions, including MG [1-3]. While research specifically focusing on the relationship between COVID-19 infection and MG is limited, there have been reports suggesting an association between the two [4,5]. Here a precipitation of life-threatening MG crisis after Covid-19 infection is reported. It is believed that the systemic inflammation and immune response triggered by a COVID-19 infection can potentially worsen or precipitate MG symptoms.
Figure 1: Patient in ICU before cardio version.
Case Report
An 85-year-old man presented with 2 years of Aside from grade 2B myasthenia with diplopia and bulbar weakness, and elevated blood pressure, he had no other medical history. A search for AChR antibodies revealed a slightly elevated titer (2.5 units). He underwent spirometry and CT of the thymus, which revealed possible residual thymus, on consultation surgery for its removal was not advised. He was treated with Mestin on 60 mg three times daily with some improvement and an alternately day steroid prednisone 25 mg regimen.
He underwent consultation with several specialists and given the scarce response to treatment was advised to do a few cycles of IVIg treatment, done in a peripheral hospital, without much improvement. The patient refused to try azathioprine or other immunosuppressant therapy.
In December of 2024, his daughter contracted a Covid-19 infection because of traveling. He was not revaccinated and underwent because of close contact a sudden Covid-19 infection with severe breathing and swallowing difficulty. On 17 December he was hospitalized for respiratory insufficiency and intubated in Intensive Care Unit in Padova Hospital.
The unit where he was had separate beds for COVID-19-infected cases: Remedivir treatment was started, and Medrol 250 mg was given with an additional IVIg cycle. on 18 December the patient was able to raise his arm(MRC strength in upper extremity muscles and grip 4/5) but was weak in lower limbs (MRC 3/5). On 23 December an extubation was tried, but failed because of bulbar weakness and a concomitant respiratory infection with dense mucus.
After another weak in the ICU, he became restless, so a second extubation was tried on January 2, 2024, which was successful. Unfortunately, he presented atrial fibrillation that was treated with digitalis and amiodarone without success, since he refused the cardio version with protocol anesthesia. On January 4 he accepted the cardio version procedure, which was successful; he was then transferred to a semi-intensive respiratory unit and discharged from the ICU.
Discussion
Myasthenia gravis (MG), patients have been predicted to have high rates of COVID-19 complications due to frequent involvement of respiratory muscles in MG and frequent use of immunosuppressive therapies. We report a rather severe case with over a fortnight of permanence in the ICU for respiratory distress after COVID-19 infection. He never developed pneumonia but was suspected to have bacterial and as per gillus pulmonary/respiratory tract infection, was for over 3 weeks markedly weak, although conscious throughout his intensive ICU stay Myasthenia gravis has been associated with higher mortality from COVID-19 compared to the general population.
Previous studies have reported that obesity, hypertension, diabetes, gender, immunosuppressants/corticosteroids, and age may be risk factors that play an important role in the development of COVID-19 in the general population [4, 5]. As expected, we found that risk factors from the general population were identified as risk factors for the impact and severity of COVID-19 in NMD patients. Interestingly, hypertension, gender, and diabetes were also recognized as common risk factors associated with the severity of COVID-19 in MS or neuromuscular cohorts.
However, in cohorts of patients with acquired NMD, treatment with corticosteroids or other immunosuppressants does not appear to be a risk factor for severe COVID-19. A look at of 15 myasthenia gravis sufferers with COVID-19 confirmed that immunosuppressive remedy did now no longer seem to motive in addition problems [7]. Using the Optum de-identified COVID-19 Electronic Health Record dataset. Primary outcomes, such a hospitalization, ventilator use, ICU admission, and death in COVID-19 patients with MG were compared with those of COVID-19 patients without MG: the subgroups of non-MG included those with rheumatoid arthritis (RA), systemic lupus, and multiple sclerosis. They concluded that COVID-19 patients with MG are more likely to be admitted to the hospital and require ICU care. Older age and patients with dysphagia had an increased risk of mortality, like in the present case. Optimal follow-up might allow the rescue of Critical MG patients, in generalized MG, therapy or physical therapy advice, diagnosis, and general follow-up should be continuous given the Covid-19 pandemic [5,6].
he worsening of NMD symptoms was reported in this patient with pre-existing respiratory impairment, and/or suffering from swallowing difficulty, and/or on long-term immunosuppressive therapy, who was classified "at high risk" for developing severe forms of COVID-19. Recent data report a 10% mortality in MG after COVID-19 infection [8], the rescue of this late-onset MG patient, gives new hope for such events.
References
-
Gagliardi D, Costamagna G, Abati E, Mauri E, Brusa R, et al. (2021) Impact of COVID-19 on the quality of life of patients with neuromuscular disorders in the Lombardy area, Italy. Muscle Nerve. 64(4):474-82
-
Tseng YH, Che TH. (2021) Care for Patients with Neuromuscular Disorders in the COVID-19 Pandemic Era, Front. Neurol. 12:607790.
-
Angelini C, Siciliano G. (2020) Neuromuscular diseases and COVID-19: advice from scientific societies and early observations in Italy. Eur J Transl Myol. 30(2):9032.
-
Guidon AC, Amato A. (2020) Covid-19, and neuromuscular disorders. Neurology. 94(22):959–9.
-
https://www.waterstones.com/book/acquired-neuromuscular-disorders/corrado-angelini/9783031067303
-
Suh J, Amato AA. (2021) Neuromuscular complications of corona virus disease-19. Curr Opin Neurol. 34(5):669-74.
-
Kim Y, Li X, Huang Y, Kim M, Shaibani A, et al. (2022) Covid-19 and Myasthenia Gravis Patients: Analysis From Electronic Health Records in the United States. Front Neurol. 13:802559
-
Thomas EV, Bou G, Barton S, Hutto S, Garcia-Santibanez R. (2023) COVID-19 infection in myasthenia gravis: Clinical course and outcomes. Muscle & Nerve. 68(2):171-75.

