mtDNA and Oral Health
Tommy Sproles III1,2 and Kuren Anderson-Steward1,2
1Department of Biology, Howard University
2Human Analytics Division, QuadGrid Data Lab
Citation: Sproles III T, Anderson-Steward K. (2024) mtDNA and Oral Health. Adv Clin Med Res. 5(2):1-7.
Received: March 25, 2024 | Published: April 15, 2024
Copyright© 2024 genesis pub by Sproles III T, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/ACMR.2024.5(2)-S3
Abstract
Much research suggests that oral health is impacted and connected to other biological factors in the body, but mtDNA’s role in oral health has been understudied. Modern insights into the mechanics of mtDNA, however, have fueled recent research on how mtDNA interacts with other biological systems. Poor dental hygiene often results in the buildup of bacteria-containing plaque on teeth that causes the release of reactive oxygen species, or ROS. In the oral cavity, it is suspected that excessive production of ROS has the capacity to damage mtDNA and trigger various oral diseases. While mitochondria naturally produce ROS by way of respiration, mutated mtDNA often results in excessive production of ROS, causing a destructive cycle of unnatural ROS production and mtDNA damage. This makes dysfunctional mtDNA the culprit of many diseases. Knowledge about mtDNA, its various components, and associated factors aids in the development of precision medicine that targets the specific mtDNA-oral health interactions of individuals instead of focusing on universal or generalized medical aids and/or cures. In this review we produce a comprehensive overview about the various oral conditions that have a significant relationship to mtDNA. A better understanding of this connection allows for more efficient innovations to be made in gene targeted oral disease therapies. Such conditions as diabetes influence oral health and its linkages with mtDNA have been reported. We also investigate the role of advanced genetic tools such as CRISPR/Cas9 to address the problematic interactions of mtDNA and oral health.
Keywords
mtDNA; Reactive oxygen species; Oxidative stress; Gingival tissue; Periodontal tissue; ATP; Carcinoma; Diabetes; PDLSCs; GACAT2; Pyruvate kinase M1/2; Precision medicine; CRISPR/Cas9.
Introduction
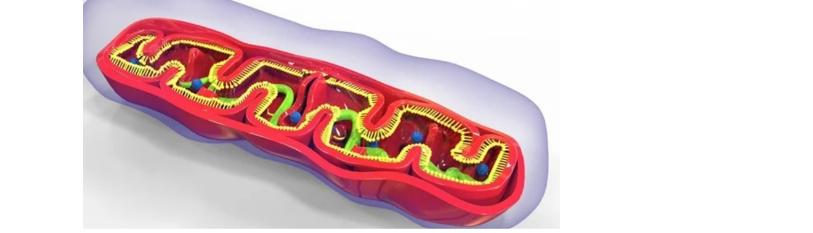
When there is an increase in reactive oxygen species within an organism, tissues are more susceptible to damage due to highly reactive molecules that can cause oxidative stress. Excess reactive oxygen species can impair numerous biological processes by inducing DNA malfunction, lipid impairment, and protein damage [3]. These damages could lead to cell dysfunction, apoptosis, and necrosis [3]. While mitochondria consistently metabolize oxygen and produce reactive oxygen species (ROS) as a byproduct, they are highly susceptible to oxidative damage [5]. ROS are synthesized because of the electron transport chain. During the electron transport chain, electrons from molecules such as NADH and FADH2 pass along a series of protein complexes. This creates a flow of electrons that generate energy used to pump electrons across the inner mitochondrial membrane. As a result, a proton gradient is created. Occasionally, electrons escape from the electron transport chain prematurely and react with oxygen molecules in lieu of reaching their destination. This can result in the formation of ROS, such as superoxide anion (02-) and hydrogen peroxide (H2O2). When reactive oxygen species levels increase, mitochondria are vulnerable to oxidation and damage to lipids, proteins, and DNA present within these organelles [1,12]. These reactions can cause impairments in the mitochondria’s ability to generate energy through a process called oxidative phosphorylation. This ultimately affects the production of adenosine triphosphate (ATP) and results in the primary source of cellular energy being compromised. Bacteria found in plaque as a biofilm often invade gingiva mucosal tissue. These bacteria trigger immune responses that activate polymorphonuclear leukocytes that produce and release ROS. Ultimately, this may result in detrimental effects on the mitochondria found in the gingiva-periodontal tissues, altering the normal mitochondrial function [3,11]. Additionally, reactive oxygen species can cause mitochondria to release harmful molecules such as cytochrome c. that trigger a cascade of events leading to apoptosis. The mitochondrion is encompassed by a double-membrane structure, one layer being the inner and the other being the outer layer, separated by an intermembrane space. This essential organelle is found within eukaryotic cells and is imperative to cells due to it being the producer of ATP. ATP is crucial for cells because it is the energy source that helps cells perform their essential functions such as protein synthesis, intracellular signaling, and muscle contraction. Being that the mitochondrion is a complex organelle in conjunction with the endosymbiotic theory stating that the mitochondria arose from free-living prokaryotes, the energy-producing organelle possesses its own set of deoxynucleic acid, DNA, called the mitochondrial DNA, shortened to mtDNA. Mitochondrial DNA is a circular-shaped structure that is solely inherited from an organism’s mother. This is due to the egg being the gamete that contributes the mitochondria to the embryo that is being produced during reproduction, while the mitochondria produced by the sperm are excluded from the developing embryo. Because mitochondria have their own DNA, mtDNA also has its own replication that is independent of the cell cycle. The independent replication of mtDNA causes a higher rate of replication in comparison to the nuclear DNA. Still, the cost of a faster replication rate is that mitochondrial DNA has a higher mutation rate located in the mitogenome than in the nuclear genome due to mtDNA lacking enzymes responsible for “proofreading” [9]. Because the mitochondria, as an entire organelle, is such a complex organism, the organelle must ensure that there is an adequate number of mitochondria within cells by way of mtDNA replication and is regulated by mitochondrial and nuclear factors.
The implications of mtDNA’s expression have become increasingly recognized in oral care. Studying the biological consequences of mtDNA on the health of the oral cavity paves the way for novel diagnostic methods that could enhance early screenings, which help identify an individual’s genetic predisposition to certain dental conditions and diseases. Dental professionals may be able to identify certain risk factors, forecast treatment outcomes, and deliver focused interventions for improved oral health with personalized treatment regimens tailored to each patient’s unique genetic information. Furthermore, through a deeper comprehension of a patient’s genetic profile, dentists can select the most appropriate drugs–anesthetics, antibiotics, pain relievers, etc.– reducing side effects and optimizing the efficacy of treatment [7]. Hence, the purpose of this study is to explore the biological maladies caused by mitochondrial processes, functional or dysfunctional, in chronic oral diseases. This study will reveal the importance of mitochondrial precision medicine in the field of oral medicine.
Methods
The most tactile way to approach this investigation was by utilizing the various databases available on the internet. Databases were found on Google Scholar through articles published within the last 25 years. All included articles had to be specifically connected to mtDNA and oral health. Articles were excluded if they were outdated, poorly written with flaws such as biases or incomplete results.
Results
The databases surveyed suggested a significant relationship between mitochondrial abnormalities and oral diseases. The databases by Damascus University that provided information on mtDNA in salivary samples found statistically significant higher mtDNA quantity in patients with head and neck squamous cell carcinomata [12,13]. These results correspond with other databases that analyze mtDNA content of cancer patients. These databases found significant differences in mtDNA levels in oral cancer patients and control subjects, leading to an impression that mtDNA increases according to the abnormality of cancer cells and tumor stage [4,6,10]. Moreover, these studies identified that mtDNA is altered by smoking, aging, tumor stage, and histopathological differentiation of leukoplakia [4,6]. Additionally, this corroborated with the data provided from a 2011 study that sampled periodontitis patients whose functional and genetic analysis showed the presence of mitochondrial dysfunction in chronic periodontitis [3].
Interestingly, a study researching oral lichen planus (OLP) susceptibility in a Chinese population discovered that mtDNA may impact the pathogenesis of OLP [15]. The researchers found that mtDNA haplogroup B4 may offer protection from the development of oral lichen planus in women [15]. These results provide a multitude of evidence that more research on the function of mtDNA as it relates to oral care is mandated. Most studies share the sentiment that while there is a historical deficit in the understanding of mtDNA behavior in patients with diseases, many recent studies have found that there is an increase in mtDNA quantity in disease-afflicted patients. Also, ROS produced by mitochondria and pathogens harm other mitochondria and periodontal tissue, and poor oral health may negatively impact mitochondria function. It is important to recognize that certain diseases, such as diabetes, appear to further aggravate periodontal disease, causing the condition to worsen immensely [14]. A 2017 study found that diabetic rodents had significantly higher amounts of alveolar bone loss and higher levels of mitochondrial dysfunction. Mitochondrial biogenesis in the rats who were diabetic with periodontitis was severely impaired (p > 0.05) [14]. It was concluded that mtDNA dysfunction in conjunction with diabetes prompted more aggressive damage done to teeth, surrounding jaw bones (such as the alveolar bone), and gums by periodontal disease. Additionally, the functionality of periodontal ligament stem cells (PDLSCs) can be linked to the inflammation of their environment [7]. PDLSCs are imperative to oral health due to the vital roles they play in helping to restore damaged periodontal ligaments, tissues, and cementum. An abundant amount of inflammation prohibits PDLSCs from fulfilling their role of differentiating into cementoblasts, a type of cell that is created by the various follicular cells surrounding the root of a tooth. Analysis of GACAT2 found that the gene significantly regulates mitochondrial function, and that its overexpression increases pyruvate kinase M1/2 (PKM1/2) expression [7]. Evidence suggest that PKM1/2 activation improves mitochondrial function by increasing mitochondrial production of ATP [7]. Extensive research conducted in this 2022 study also found that the overexpression of the GACAT2 gene could potentially reverse inflammation-induced mitochondria functional damage and the failure of PDLSCs differentiation into cementoblasts in an inflammatory environment [7].
Discussion
MtDNA concentration could be used as a biomarker of maladies found in the oral cavity. Additionally, mtDNA found in oral tissues are likely damaged by ROS, carcinoma, age, and smoking that ultimately lead to its malfunction. With advancements in gene-editing technology and dental research, the use of CRISPR/Cas9 shows promise to relieve or completely delete unfavorable mutations caused by these damages. This is imperative to the movement of personalized medicine in dentistry. Better comprehending the genome’s relation to oral health can pave the way for the manufacture of treatments that target inherited medical conditions, customizable to each patient. While various factors such as environment and daily routine habits play a large role in a patient’s potential remedy, it is also important to acknowledge that the differences within a molecular level should be assessed as well to build a unique remedy that aids patients.
Understanding the molecular factors that play a role in tooth and gum degeneration can help curate medicinal practices for the by-products of common diseases, such as diabetes. For patients with diabetes, it is important to ensure that adequate insulin is being produced and the body is receiving the insulin properly. If this is not controlled, it could lead to increased levels of glucose in one’s saliva, promoting higher levels of bacteria that cause cavities, dental caries, and gum disease. This is due to the bacteria, such as streptococci that thrive in this environment, producing acid that erodes tooth enamel, eventually leading to tooth decay and gum disease if proper precautions are not taken. Enriching the bacterial environment increases the production of ROS, increasing the likelihood of mutations to mtDNA. Better understanding how ROS contributes to the mutagenesis of mtDNA, and how mtDNA dysfunction often leads to oral disease could allow for more efficient care to individuals who suffer from diseases like diabetes.
Although the lack of data on mtDNA’s direct contribution to the pathogenesis of oral diseases caused a lot of difficulty in finding concise answers on the correlation between mtDNA and oral health, this preliminary study indicated the importance of mitochondrial awareness in dental research. Researchers are discovering new ways to diagnose dental conditions early by studying how mtDNA affects oral health. This enables timely interventions and more effective treatment strategies for people who might have a genetic predisposition to certain oral diseases. With more knowledge of mtDNA’s impact on oral health, oral care providers may be able to analyze genetic markers to identify specific risk factors, predict treatment outcomes, and provide targeted interventions for better oral health [8]. Dentists may be able to better understand a patient’s genetic profile to choose the right medications, which reduces side effects and makes treatment more effective [8]. Personalized medicinal treatment could minimize adverse reactions and maximize treatment effectiveness. By exploring the impact of mitochondrial processes on chronic oral diseases, the innovations of precision medicine can be embraced by the dental community, and the field of dentistry can evolve with the current medicinal innovations that the upcoming years will bring.
Declarations
Ethics approval and consent to participate All data discussed in this paper are from published databases.
Consent for publication
Both authors of this paper agree to its submission for publication consideration.
Availability of data and materials
All databases consulted in this paper are already in the public domain.
Competing interests
The authors declare no competing interests.
Funding
This work is supported by the Division of Engagement and Outreach, All of Us Research Program, National Institutes of Health under award number 1OT20D028395-01 and a small grant from QuadGrid Data Lab, Bethesda, MD.
Authors' contributions
The paper was conceived, written, and reviewed by both authors. Both authors participated in the approval of the final version.
Acknowledgements
The authors developed this paper for the Special Issue of Advances in Clinical and Medical Research.

