Comparative Study of Rebamipide & Betamethasone in Managing Stomatopyrosis in Oral Submucous Fibrosis (OSMF) Patients
Asdullah1*, Rajendra Kumar Tiwari1, Pradhuman Verma1, Kauser J Khwaja1 and Anshul Aggarwal1
1Department of Oral Pathology; Oral Medicine & Radiology, Dr. Z A Dental College & Hospital, A.M.U Aligarh, India
*Corresponding author: Md Asdullah, Department of Oral Pathology; Oral Medicine & Radiology, Dr. Z.A Dental College & Hospital, A.M.U Aligarh, India.
Citation: Asdullah M, Tiwari RK, Verma P, Khwaja KJ, Aggarwal A. (2021) Department of Oral Pathology; Oral Medicine & Radiology, Dr. Z A Dental College & Hospital, A.M.U Aligarh, India. J Oral Med and Dent Res. 2(2):1-06.
Received: August 17, 2021 | Published: September 20, 2021
Copyright© 2021 genesis pub by Asdullah Md, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Introduction: The incidence of Oral Sub Mucous Fibrosis (OSF) is commonly seen in the Indian subcontinent. It affects individuals of all age groups. It is a potentially malignant disorder caused almost exclusively by the use of the smokeless form of tobacco products. The malignant transformation rates vary from 3 to 19%. The Standard of Care (SOC) in managing OSF includes habit cessation, intralesional steroid and hyaluronidase injections, and mouth opening exercises.
Objectives: To evaluate the efficacy of rebamipide to reduce the oral burning sensation associated with OSMF as compared to conventional Betamethasone intralesional injection.
Material and Methods: Consent was taken after detail briefing about the study to the patients. Patients were divided into two groups of 15 each using a random sampling method. Patients in the rebamipide group (group I) were prescribed 100 mg tablets of rebamipide thrice a day for 21 days. The other 15 patients (group II) were given SOC, intralesional betamethasone injection 4 mg/mL once a week for 4 weeks. Visual analog scale (VAS) with 11 points (0-10) was used to assess burning sensation in the first visit, and change in the burning sensation was assessed after every 7th day on VAS in both the groups.
Results: The improvement in the VAS score in each visit was significant (p < 0.05) in the 1st, 2nd, 3rd, and 4th visit. The VAS score between the 4th and 5th visit failed to reach a statistically significant level (p > 0.05). The VAS score was significantly different between the rebamipide and betamethasone group (p > 0.05) in third & fourth visits.
Conclusion: Our results showed that rebamipide was equally efficacious if not better than the betamethasone intralesional injections.
Keywords
Betamethasone; Management; Oral submucous fibrosis; Rebamipide
Introduction
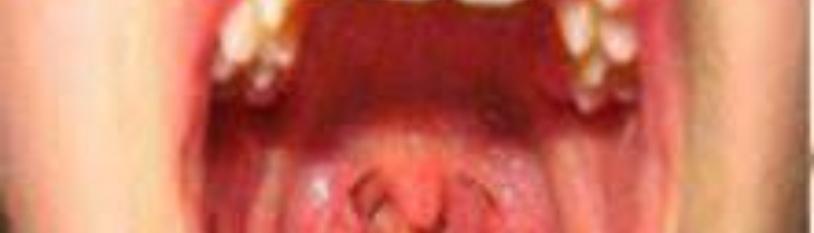
The incidence of Oral sub mucous fibrosis (OSF) is commonly seen in the Indian subcontinent.It affect individuals of all age groups. It is a potentially malignant disorder caused almost exclusively by the use of smokeless form of tobacco products. The malignant transformation rates vary from 3 to 19% [1-3]. Progressive debilitating symptoms caused by oral sub mucous fibrosis affecting the oral cavity, such as burning sensation, loss of cheek elasticity, restricted tongue movements, and limited mouth opening. Injuries due to continuous local irritation caused by gutkha, paan masala or areca nut can lead to oxidative stress, chronic inflammation and cytokine production. Oxidative stress and subsequent Reactive Oxygen Species (ROS) generation induces cell proliferation, cell senescence, or apoptosis, depending upon the amount of ROS produced. Chronic exposure leads to preneoplastic lesions in the oral cavity which subsequently transform into cancerous [4]. Oral sub mucous fibrosis is an irreversible condition and the management strategies are reducing the symptoms. Habit cessation, intralesional steroid and hyaluronidase injections, and mouth opening exercises come under The Standard of Care (SOC) in managing OSF. It affects the oral cavity and in severe forms can involve the pharynx. The characteristic symptoms of burning sensation and stiffness of the oral mucosa is estimated that 33% of men and 18% of women use smokeless form of tobacco in India [5]. Carcinogenesis occurs by generation of ROS, which act by initiating lipid peroxidase. In OSF, lipid peroxidase was found to increase according to the severity of the disease [6]. Rebamipide anti-inflammatory action is due to the reduction of inflammatory interleukin (IL)-6 and IL-8, reduction of neutrophil migration, and scavenging of free radicals [7].
Aim & Objective
To evaluate the efficacy of rebamipide [2-(4-chlorobenzoyl) amino]-3-(2-oxo-1Hquinolin-4-yl) propanoic acid], essentially a mucosal protective agent, to reduce the oral burning sensation associated with OSMF as compared to coventional Betamethasone intralesional injection.
Material and Methods
After obtaining the institution ethical committee approval, this prospective clinical study was undertaken among OSMF patients reporting to the OPD of department of oral Medicine & Radiology.
Inclusion & Exclusion Criteria
The inclusion criteria included all clinically diagnosed immune-competent OSMF patients complaining of burning sensation in the mouth. Patients who were already taken treatment for OSMF, pregnant or nursing mothers, and those with known systemic illnesses or history of drug allergies were excluded from the study.
Methodology
After providing information about the study and obtaining consent, these individuals were divided into two groups of 15 each using random sampling method. Patients in the rebamipide group (group I) were prescribed 100 mg tablets of rebamipide thrice a day for 21 days. The other 15 patients (group II) were given SOC, intralesional betamethasone injection 4 mg/ml once a week for 4 weeks. Visual analog scale (VAS) with 11 points (0-10) was used to assess burning sensation in the first visit, and change in the burning sensation was assessed after every 7th day on VAS in both the groups. Patients were followed up for 4 weeks and were advised to report adverse events if any. During the follow-up visit, number of tablets remaining was evaluated to ensure compliance to therapy.
Results
Mean & standard deviation of the evaluation of burning sensation by VAS score was calculated and comparison between the rebamipide and betamethasone group was done by using paired t-test (Graph pad method). The age range of the study population was 19 to 65 years, with a mean age of the study population being 32.2 ± 10.09 years. The rebamipide group had 13 males and 2females, and the SOC (betamethasone) group had 14 males and 1 female. The VAS scores were evaluated for both the groups on 1st, 7th, 14th, 21st and 30th day.
|
Type of Treatment
|
Visit
|
VAS Mean
|
Standard Deviation
|
|
Rebamipide (gp-1 of 15)
|
First |
4.7 |
1.94 |
|
Second |
3.2 |
1.68 |
|
|
Third |
1.8 |
1.68 |
|
|
Fourth |
0.8 |
0.91 |
|
|
Fifth |
0.8 |
0.91 |
|
|
Betamethasone (gp-11 of 15)
|
First |
5.3 |
1.70 |
|
Second |
3.9 |
1.37 |
|
|
Third |
3.1 |
1.28 |
|
|
Fourth |
2.1 |
1.52 |
|
|
Fifth |
1.6 |
1.07 |
Table 1: summarizes the mean VAS scores of burning sensation in both the groups during their weekly follow-up visit. Patients who were in rebamipide group the burning sensation reduced from 4.7 to 0.8 on day 30. The burning sensation Patients in betamethasone group, reduced from 5.3 to 1.6 on day 30.
The improvement in the VAS score in each visit was significant (p < 0.05) in the 1st, 2nd, 3rd, and 4th visit. The VAS score between the 4th and 5th visit failed to reach a statistically significant level (p > 0.05). The VAS score was significantly different between the rebamipide and betamethasone group (p > 0.05) in third & fourth visit (Table 2).
|
|
t value
|
df value
|
P value
|
|
First |
t=0.90 |
df=28
|
P=0.3753
|
|
Second |
t=1.25 |
df=28
|
P=0.2214
|
|
Third |
t=2.38 |
df=28
|
P=0.0242
|
|
Fourth |
t=2.84 |
df=28
|
P=0.0083
|
|
Fifth |
t=2.38 |
df=28
|
P=0.024
|
Table 2: Statistical comparative analysis between group 1 & group 11.
Discussion
Various treatment modalities had been tried with varying results like vitamin A supplementation, lycopene, pentoxifylline, hyaluronidase, corticosteroids, and placental extracts, all targeted at reducing inflammation for symptomatic relief to the patient [8-12]. The Complete cure of the disease has not been possible till date. Intralesional injections of steroids though very popular are purely palliative and have no curative value. It is also believed that repeated injection of the drug may further lead to fibrosis and associated trismus. Patient compliance is also poor due to the repeated painful intraoral injections. Rebamipide reduces or blocks the ability of human mast cells to release cyclic adenosine monophosphate phosphodiesterase, an inflammatory mediator. It also blocks proinflammatory substances and the production of substances that cause inflammatory reactions [13]. Rebamipide has been used as a gastroprotective drug and has demonstrated its ulcer healing properties in animal as well as human studies. It stimulates prostaglandin synthesis in the mucosa and improves the speed and the quality of ulcer healing [14-15]. Rebamipide has been used effectively in managing aphthous stomatitis and Behcet’s disease [16].
Patient compliance to rebamipide therapy was assessed by asking the patient to carry the tablet strip with them during their weekly follow-up. All patients in the group completed the treatment. Significant reduction in burning sensation was seen from the initial visit to the 1-month follow-up, and none of the patients had worsening of the fibrosis or any adverse drug reaction.Our finding are consistant with study conducted by Joanna B, et al. ‘’Rebamipide to manage stomatopyrosis in oral submucous fibrosis’’ [1]. It is further suggested that similar study with large sample size should be carried out to prove authenticity of efficacy of this drug in managing stomatopyrosis in OSMF.
Conclusion
Our results showed that Rebamipide was equally efficacious if not better than the Betamethasone intralesional injections. Lack of iatrogenic fibrosis and better patient compliance and caused by repeated mucosal injections make rebamipide a painless alternative to alleviate burning sensation in patients with OSMF. More studies with large subjects should be carried out for more authenticity of findings and scientific basis of its clinical implications.
References
- Baptist J, Shakya S, Ongole R. (2016) Rebamipide to Manage Stomatopyrosis in Oral Submucous Fibrosis. J Contemp Dent Pract. 17(12):1009-12.
- Sarode SC, Sarode GS. (2013) Better grade of tumor differentiation of oral squamous cell carcinoma arising in background of oral submucous fibrosis. Med Hypotheses. 81(4): 540-3.
- Chen HM, Hsieh RP, Yang H, Kuo YS, Kuo MY, et al. (2004) HLA typing in Taiwanese patients with oral sub mucous fibrosis. J Oral Pathol Med. 33(4):191-9.
- Jeng JH, Wang YJ, Chang WH, Wu HL, Li CH, et al. (2004) Reactive oxygen species are crucial for hydroxychavicol toxicity toward KB epithelial cells. Cell Mol Life Sci. 61(1):83-96.
- World Health Organization. (2009) Regional office for South-East Asia global adult tobacco survey (GATS): India country report. New Delhi: WHO-SEARO.
- Gupta S, Reddy MV, Harinath BC. (2004) Role of oxidative stress and antioxidants in aetiopathogenesis and management of oral submucous fibrosis. Indian J Clin Biochem. 19(1):138-41.
- Kim H, Seo JY, Kim KH. (2000) Inhibition of lipid peroxidation, NF-kB activation and IL-8 production by rebamipide in Helicobacter pylori-stimulated gastric epithelial cells. Dig Dis Sci. 45(3):621-28.
- Lai DR, Chen HR, Lin LM, Huang YL, Tsai CC. (1995) Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10-year experience with 150 cases. J Oral Pathol Med. 24(9):402-6.
- Rajendra R, Rani V, Shaikh S. (2006) Pentoxifylline therapy: a new adjunct in the treatment of oral submucous fibrosis. Indian J Dent Res. 17(4):190-8.
- Kumar A, Bagewadi A, Keluskar V, Singh M. (2007) Efficacy of lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 103(2):207-13.
- Lin HJ, Lin JC. (2007) Treatment of oral submucous fibrosis by collagenase: effects on oral opening and eating function. Oral Dis. 13(4):407-13.
- Kakar PK, Puri RK, Venkatachalam VP. (1985) Oral submucous fibrosis-treatment with hyalase. J Laryngol Otol. 99(1): 57-9.
- Shimoyama T, Fukuda S, Liu Q, Fukuda Y, Nakaji S, et al. (2003) Characteristics of attenuating effects of rebamipide, an anti-ulcer agent, on oxidative bursts of human neutrophils. J Pharmacol Sci. 91(2):153-7.
- lijima K, Ichikawa T, Okada S, Ogawa M, Koike T, et al. (2009) Rebamipide, a cytoprotective drug, increases gastric mucus secretion in human: evaluations with endoscopic gastrin test. Dig Dis Sci. 54(7):1500-07.
- Naito Y, Kuroda M, Mizushima K, Takagi T, Handa O, et al. (2007) Transcriptome analysis for cytoprotective actions of rebamipide against indomethacin-nduced gastric mucosal injury in rats. J Clin Biochem Nutr. 41(3):202-10.
- Matsuda T, Ohno S, Hirohata S, Miyanaga Y, Ujihara H, et al. (2003) Efficacy of rebamipide as adjunctive therapy in the treatment of recurrent oral aphthous ulcers in patients with Behçet's disease: a randomised, double-blind, placebo-controlled study. Drug RD. 4(1):19-28.

