Shervin Molayem1*, Carla Cruvinel Pontes2
1Periodontist; Private Practice, Director of the Mouth Body Research Institute, Los Angeles, California, USA
2Researcher, Mouth-Body Research Institute, Cape Town, South Africa
*Corresponding author: Periodontist; Private Practice, Director of the Mouth Body Research Institute, Los Angeles, California, USA.
Citation: Molayem S, Pontes CC. (2023) Face Masks to Prevent COVID-19: A Critical Appraisal of Current Evidence. J Oral Med and Dent Res. 4(1):1-12.
Received: January 23, 2023 | Published: February 06, 2023
Copyright© 2023 genesis pub by Molayem S, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non-Commercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JOMDR.2023.4(1)-31
Abstract
Background: Face-masks have been one of the pillars for reducing the spread of COVID-19 by limiting exposure to SARS-CoV-2. However, the effectiveness of face-masks has frequently been the focus of debate among scientists and the general public.
Types of studies reviewed: This mini-review presents a critical analysis of factors that influence the effectiveness of face-masks on disease transmission, their benefits and side effects for adults and children, and their impact on the environment. These topics are summarized based on the most relevant research available in the literature.
Results: The mask type, fitting, behavior, and hygiene affect filtration efficiency. Cloth masks present low protection, and poor hygiene can increase the risk of infection. Surgical masks present moderate protection, with respirators such as N95 presenting the highest protection. Prolonged use of face masks and respirators can alter respiratory patterns, with the potential to cause side effects in adults and children.
Practical implications: In the context of disease transmission, surgical and cloth masks protect for minutes, and respirators for hours. The decision to wear a mask or not should consider comorbidities, well-being, and the nature of social interactions. By weighing risks and benefits, each individual should be able to make a conscious, informed decision.
Keywords
Mask wearing; COVID-19; Viral transmission; Filtration efficiency of face-masks.
Introduction
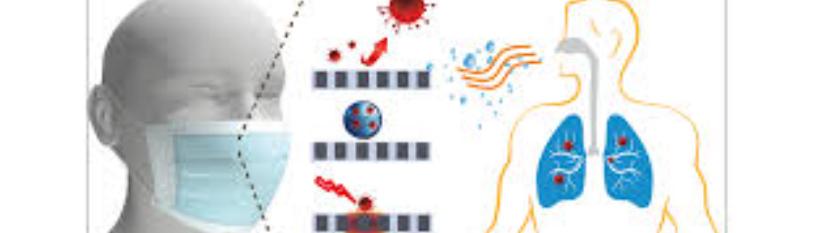
The foundation for reducing the spread of the corona virus disease has been based on limiting exposure to SARS-CoV-2 through face masks, social distancing, and hand hygiene. Similarly to other respiratory viruses, SARS-CoV-2 spreads through airborne droplets that can reach the mucosa in the oral cavity, nasal cavity, or the eyes, with the potential to infect host cells and cause disease [1]. Despite the contribution of face masks to the reduction of viral transmission in community settings, their actual effectiveness has frequently been the focus of debate among scientists and the general public [2].
According to the Centers for Disease Control (CDC), the primary function of face masks is to decrease the wearer's emission of infectious particles into the environment. At the height of the pandemic, mask mandates helped decrease the incidence of COVID-19 [3]. The uses of medical-grade masks and respirators in hospitals, and healthcare facilities have played an essential role in protecting health professionals from SARS-CoV-2. However, the efficiency of other mask types in public settings has been questioned [4]. Other mask-related issues, such as mask handling and hygiene, have often been neglected despite their potential for lowering mask effectiveness. Lack of adequate care can turn face-masks into sources of bacterial and fungal infections in the skin, respiratory and digestive tracts, which can aggravate COVID-19 [5].
As the CDC relaxed COVID-19 guidelines to promote a "live with the virus" approach, whether to wear a face mask or not is now a personal choice [6]. As of August 2022, a simple search for systematic reviews on the use of face masks for preventing COVID-19 shows forty-six results on Pubmed. The extensive literature on the topic makes it challenging to draw clear conclusions.
Many different masks are available, including homemade and manufactured cloth masks with different fabrics, bandanas, gaiters, medical surgical masks, and respirators, such as the N95 model. During the pandemic, several countries recommended wearing masks in public without distinction on mask types. The scarce supply of personal protective equipment (PPE), higher medical masks, and respirator costs likely propelled the public towards cloth masks [7]. However, the current low mortality rates, reduced pressure on healthcare systems, and sufficient supply of medical face-masks call for a data-focused questioning about mask-wearing and viral transmission [8]. The efficiency of face masks depends on multiple intrinsic factors, such as type of mask, fitting, filtration capacity, fabric microstructure, and thickness, as well extrinsic factors, such as duration of social interaction and type of environment [4].
Despite the lower disruption of daily lives by COVID-19 and the shift towards an endemic disease, it still requires vigilance. This mini-review aims to critically analyze the factors that influence the effectiveness of face mask wearing on disease transmission, their benefits and side effects for adults and children, and their impact on the environment. This article provides a scientific discussion to enable readers to make informed decisions.
Technical Principles of Face-Masks as Protective Barriers against SARS-CoV-2
A few concepts used in aerosol science are helpful to understand better the basic parameters involved in mask efficacy. SARS-CoV-2 has about 0.1 µm in diameter and it travels through the air in aerosols. Aerosols, also known as droplet nuclei, originate from larger respiratory droplets that have evaporated, with sizes up to 5 µm. These minor inhalable particles carrying the virus are the most significant transmission source, as they can stay in the air for long periods and pass through gaps and pores [9]. The filtration effectiveness of masks cannot be quantified simply by comparing the size of aerosol particles to the size of mask pores. The reasons for that include the 3D and electrostatic aspects of the fabric material and aerosol particles' route in motion [10-11]. Studies on face masks evaluate the emission of particles (protection of others) and the inhalation of particles (protection from others) [12].
Factors Affecting Face Masks Effectiveness
Cloth masks, surgical masks, and respirators constitute the most common protective barriers. Cloth masks include a variety of commercial or homemade fabric masks that considerably vary in material, construction, fit, and design. Natural or synthetic textiles with varying thread counts per inch have been used, including cotton, cotton blends, silk, flannel, polyester, spandex, nylon, and chiffon. Cloth masks are unsuitable in healthcare settings due to their lack of standardization [13].
Surgical masks are typically made of 3 layers of non-woven fabric, mostly polypropylene, and follow rigorous design standards. They can also be made from other thermoplastic polymers such as polyester, polystyrene, polyethylene, or polycarbonate. The outermost layer is leak proof, the inner layer is a high-density filter, and the inner layer is in direct contact with the skin [14].
Respirators constitute specialized filtering devices with a convex cap shape composed of 4 layers of polypropylene. The most well-known respirator in the US is the N95, whose manufacturing is controlled by the National Institute for Occupational Health and Safety (NIOSH), the CDC, and the Occupational Safety and Health Administration (OSHA). Respirators are designed to create a seal around the nose and mouth [15].
Filtration Efficiency
Filtration efficiency is defined as the protection masks offer the wearer when exposed to potentially infected people [16].
Cloth masks: Despite their popularity, cloth masks present low filtration efficiency of aerosols, varying between 2-38% due to their large pores. Cloth masks composed of three or more layers present higher filtration ability [17]. After four wash and dry cycles, their filtration efficiency can lower by up to 20% [18]. Clapp and coworkers reported that folded cotton bandanas had about 50% filtration efficiency, while a single-layer gaiter composed mainly of polyester had about 38% filtration efficiency despite the tighter fit. Having a nose bridge and a filter increases the filtration effectiveness of cloth masks [19]. Emission of large droplets can be reduced through cloth masks; however, protection against inhalation or emission of smaller aerosol particles is limited [20]. Cloth masks are half as efficacious as N95 and 25% less effective than surgical masks [21].
The type of cloth impacts blockage of particles, with thicker fabrics presenting higher filtration efficacy, estimated at 40% for towels, 20-40% for sweatshirts, 10-20% for cotton, and 10% for t-shirts. Multi-layered masks made with cotton or tightly woven fabrics that do not allow passage of light when held up to bright light and fit adequately with no leaks can increase protection [22-23]. The bottom line is that cloth masks present low protection against aerosols, with one-layer masks being the most ineffective. Thus, when wearing a cloth mask, even a limited number of viral aerosol particles can pass through the cloth and cause infection [22].
Surgical masks: Surgical masks with elastic ear loops present a filtration efficiency of 38.1%. For those with tie strings, it increases to 71.5% due to minimized gaps. Clapp et al. recommend tying ear loops and tucking side pleats for increased protection. Surgical masks can provide moderate protection against COVID-19 given that their fit is optimized [19].
Respirators: As their name implies, N95, N99, and N100 respirators block at least 95%, 99%, and 99.97% of aerosol particles, respectively [19]. These respirators are the most efficient barriers against viral transmission, which is why the CDC recommends their use to healthcare personnel during aerosol-producing procedures [24-25].
Porosity
Cloth masks present 82% porosity. Higher porosity means air is allowed in and out, which translates into higher breathability. It also means a higher risk for the movement of particles. The pore size varies from 80 to 800 µm in textile masks, depending on fabric type [26]. Medical or surgical masks present intermediate porosity (77%) and breathability [26]. N95 masks present the lowest porosity (65%) and breathability. It presents the smallest pores (about 30 µm) and the highest fiber density. These are the main reasons for their superiority in aerosol filtration [26].
Mask Hygiene
Human saliva presents a high concentration of microorganisms, constituting a biosafety issue during prolonged use of face-masks. Furthermore, skin and upper respiratory microorganisms can also colonize face masks. They constitute fertile grounds for bacterial growth, given the high temperature and humidity conditions. Bacteria in the mask can be inhaled or colonize the skin under the mask [27]. Cotton textiles are particularly prone to microbial contamination and growth due to their ability to retain moisture. Thus, reusable masks require adequate disinfection before safe reuse; otherwise, they increase the risk of infection [28].
A microbial study of cloth and surgical masks revealed frequent accumulation of bacterial pathogens after 4 hours of mask use, including antibiotic-resistant microorganisms on surgical masks and more intensely in cotton masks. In the same study, a survey on mask hygiene reported that only 8% of surgical mask wearers used it once, and 21% of cotton mask wearers cleaned it daily [27]. The authors suggest that surgical masks are better than cotton masks if worn over four hours due to their lower bacterial counts. Furthermore, hand washing before and after handling a mask is essential. Cloth masks require daily washing at 140oF with a detergent, boiling, or ironing [27]. They should be kept moist-free and clean. Harsh chemicals and bleach should be avoided [29].
Surgical masks and respirators are intended for single use. Due to the risk of lower filtration efficacy, reprocessing, extended use, or reuse of these barriers is not recommended. In the case of supply shortage, ultraviolet germicidal irradiation and hydrogen peroxide offers the least disruptive disinfection methods.30Soap and water, microwave irradiation, and alcohol are not suggested for mask cleaning, given the risk of compromising filtration. If the surgical mask or respirator becomes soiled or damaged, or breathing becomes challenging, it should be safely discarded inside a plastic bag and replaced [31].
Type of Environment
The amount of aerosol particles in the air depends on the concentration of people and the type of environment. Crowded indoor spaces present a higher concentration of inhalable particles resulting from breathing, speaking, or singing. These particles can move through air currents and diffusion; thus, social distancing alone might not avoid disease transmission. The longer a person stays in a shared space, the more particles are likely to be inhaled. Sharing a well-ventilated space with fewer people for shorter periods decreases the concentration of particles and risk for contamination with respiratory viruses such as SARS-CoV-2 [22].
Duration of Exposure and Fitting
Brosseau et al. presented the estimated degree of protection conferred by different types of masks concerning the time needed for an uninfected person (the receiver) to reach an infectious viral dose from an infected person (Table 1). The author presents different scenarios according to the percentage of inward leakage, considering that a typical cloth mask has 75%, a typical surgical mask has 50%, non-fit-tested N95 has 20%, and fit-tested N95 has 10% inward leakage [32].
|
-
|
Receiver
|
|
No Mask
|
Cloth Mask
|
Surgical Mask
|
N95
|
N95 fit-tested
|
|
Source
|
% Outward Leakage
|
100%
|
75%
|
50%
|
20%
|
10%
|
|
No mask
|
100%
|
15 min
|
20 min
|
30 min
|
1.25 hr
|
2.5 hr
|
|
Cloth mask
|
75%
|
20 min
|
26 min
|
40 min
|
1.7 hr
|
3.3 hr
|
|
Surgical mask
|
50%
|
30 min
|
40 min
|
1 hr
|
2.5 hr
|
5 hr
|
|
N95
|
20%
|
1.25 hr
|
1.7 hr
|
2.5 hr
|
6.25 hr
|
12.5 hr
|
|
N95 fit-tested
|
10%
|
2.5 hr
|
3.3 hr
|
5 hr
|
12.5 hr
|
25 hr
|
Table 1: Time to infectious dose from an infected source to an uninfected receiver according to the type of mask worn by each, presented in minutes (min) and hours (hr). Published by the Center for Infectious Disease Research and Policy (CIDRAP) in 2021, reproduced with permission from CIDRAP.
In the worst-case scenario, in the absence of facemasks, it takes 15 minutes for the receiver to get an infectious dose. If the source and the receiver wear cloth masks, the time increases to 26 minutes and to about one hour if both wear surgical masks. For the best-case scenario, if the source and the receiver wear an N95 respirator, it would take over 12 hours for the latter to reach an infectious viral dose. Fit-tested N95 for both source and receiver increases the time to infectious dose to 25 hours [32]. A fit test evaluates the comfort, fitting, and protection provided by a respirator, being required to decrease leakage and risk for infection in workplaces that involve exposure to infective agents [33].
Fit tests have highlighted the importance of fit to avoid leaks and gaps and maintain protection against viral infections. Therefore, Gandhi and Marr suggest that high-quality, tight-fitting masks are preferred in crowded indoor places. Alternatively, a tight-fitting cloth mask can be worn over a surgical mask to decrease leakage [34].
Adverse Effect of Face Mask Wearing
With COVID-19 mortality decreasing in most countries, the real question is if masks are needed. While masks are required as PPE for healthcare providers, in most instances, masks are optional for asymptomatic individuals in the US [35]. The prolonged and repeated mask use has been linked to multiple side effects [36]. Face masks cover facial expressions and muffle sounds, thus hindering interpersonal communication [37].
Pressure on the face and headaches have also been reported as side effects of prolonged mask-wearing, particularly with N95 respirators. After one and four hours of wearing a N95 mask, attention deficit, lower concentration, and headaches were reported by Ipek and colleagues [38].
Multiple studies report lower oxygen (hypoxia) and higher carbon dioxide (CO2) levels (hypercapnia) in the air under the mask and in the blood during the use of surgical masks and N95 respirators, as summarized in the review by Kisielinski [36]. When worn during physical exercise, cloth and surgical masks and N95 respirators were linked with increased heart rate, breathing difficulties, exhaustion, heat, and itchiness in the face. Hypoxia and hypercapnia can cause psychological and neurological effects, such as fatigue, disorientation, confusion, decreased thinking capacity, psychomotor abilities, and impaired cognition [36]. It has been estimated that N95 respirators lower gas exchange by 37%, possibly triggered by a 128% increase in breathing resistance and an 80% increase in dead space volume. Not all inhaled air is subjected to gas exchange. Dead space describes the volume of air that is not exchanged after inhalation. Thus, repeated use of masks over prolonged periods may lead to shifts that contribute to disease [39-40].
In patients presenting severe chronic obstructive pulmonary disease (COPD), N95 respirators can increase the risk for respiratory failure and should be removed immediately if headache, dizziness, or dyspnea develops [41-42]. Caution is also needed for patients with end-stage kidney disease and pregnant women due to their potential to influence cardiopulmonary function [43].
Dermatological conditions have also been described as a consequence of mask-wearing. The high humidity and temperature under a mask increase sebum production, altering the skin barrier function. As a result, existing skin conditions can worsen, and new conditions can develop, such as dermatitis, acne, desquamation, rosacea, eczema, and urticaria [44].
Changes to the oral mucosa have also been described as an adverse effect of mask-wearing. The most common conditions include dry mouth, gingivitis, halitosis, and candidiasis [45-48]. Those changes have been attributed to increase mouth breathing triggered by breathing resistance, which lowers salivary flow and soft tissue dehydration [36]. Frequent reuse, incorrect use, and low filtration efficiency of cloth masks increase the risk of infection due to the beneficial conditions for microbial growth, as discussed in a previous session [28].
Face masks can provide a false sense of security, leading to a disregard for other mitigation strategies. Individuals wearing masks tend to talk louder and move closer to one another during conversations due to their impact on communication, thus increasing the risk of viral transmission [49].
Benefits of Mask Wearing
There is enough evidence to suggest that respirators efficiently reduce the spread of SARS-CoV-2 and prevent infection [50]. However, this applies to a lesser degree to surgical masks and even less so to cloth masks [29]. At the current stage of COVID-19, face-masks can be beneficial to lower the chance of transmission among the elderly, immunocompromised, and high-risk patients despite the risk of adverse side effects. Patients with heart disease, diabetes, hypertension, obesity, cancer, chronic lung, liver or kidney disease, cystic fibrosis, cognitive disorders, HIV, and disabilities are more likely to develop severe COVID-19 [51].
Courtney & Bax suggest that the high humidity created by face masks around the nose and the mouth might protect against COVID-19. After viral particles reach the respiratory tract, the moisture would favor mucociliary clearance and the immune response, possibly decreasing the risk of infection [52]. Nevertheless, this possible beneficial effect has only been discussed in theory.
Face-Masks and Children
While the World Health Organization (WHO) recommends mask-wearing from the age of 5, [53] and the European Centre for Disease Prevention and Control from the age of 12, [54]the US authorities recommend it for children two years and older [55]. Currently, there is a lack of research on the safety of masks for children. Thus, age-appropriate evidence-based recommendations are lacking [56].
Children are physiologically more vulnerable to the side effects of prolonged use of facemasks than adults due to their higher oxygen demand, smaller airways, and higher susceptibility of the central nervous system to hypoxia. Breathing difficulty and altered respiratory physiology are frequently reported in children wearing masks, which can cause anxiety [57]. In younger children, in particular, masks affect non-verbal communication, speech, social interactions, and emotional bonding, ultimately affecting their brain development [49].
From a filtration efficiency point of view, respirators are the only ones designed to protect against aerosols [47,50]. Nevertheless, their once-off nature, lack of fit on pediatric faces, and adverse effects make them impractical for children. Another point to consider is that young children typically cannot maintain masks correctly for long periods, such as during school hours [58]. Children with cognitive, asthma or respiratory impairment may have a lower tolerance to face-masks. For children with greater risk for COVID-19 due to immunosuppressive or chronic disease, quality masks can be required if community transmission increases [59].
Children are at lower risk of getting infected and developing severe COVID-19 than adults, possibly due to reduced expression of angiotensin-converting enzyme 2 (ACE2) receptors in their nasal cavities [60,61] Thus, the consequences of masks in children, including discomfort, social issues, impaired interpersonal communication, and physiological respiratory changes, should be carefully evaluated against their benefits [62].Children's physical, emotional, and developmental should be prioritized now that the world is learning to live with COVID-19. Asymptomatic children under 12 should not be required to wear masks [54]. However, new variants can emerge in the ever-changing COVID-19 scenario, requiring tighter community mitigation strategies. Current CDC guidelines include wearing a high-quality mask ten days after exposure to COVID-19 or a positive test. This approach suggests that, at this point, masks can help speed up the return to school for kids exposed or infected with SARS-CoV-2 [9].
Environmental Impact of Mask-Wearing
COVID-19 has undeniably impacted the environment. The disposal of face-masks is one of the environmental challenges fueled by the pandemic. It is estimated that 7,200 tons of medical waste are produced daily due to COVID-19, significantly due to disposable mask waste [63]. Most surgical masks and respirators contain polypropylene or other plastic derivatives, which are not biodegradable. Thus, globally, tons of mask plastic waste ends up in the oceans, negatively affecting the environment, global economy, and life on the planet. Furthermore, used masks can be infectious, potentially affecting public health and disease transmission. Recycling, producing effective reusable masks, and creating biodegradable disposable masks are proposed solutions to decrease the environmental toll of face masks [64].
Take Home Message
- Under the current circumstances, the decision to wear a face-mask is primarily individual, as mandates are no longer in place. According to the discussion in the previous sections, the main factors related to mask-wearing are summarized below:
- Respirators are designed to filter micro particles such as those involved in COVID-19 transmission efficiently. However, they present low breathability and high cost [24].
- Surgical masks offer moderate filtration ability and better breathability depending on their fit [24]. Cloth masks present good breathability with varying degrees of filtration. Most commonly used single-layer cloth masks offer low protection. Reusing cloth masks without proper hygiene can increase the risk of infection [13].
- Personal factors such as previous exposure to the virus, chronic conditions that increase the risk of severe COVID-19, and psychological well-being should be considered [32].
- The nature (indoor or outdoor, ventilation, number of people, etc.) and duration of social interactions affect the risk of infection, with short-duration outdoor events presenting the lowest infection risk [32].
- Loose fitting results in gaps, decreasing the filtering ability of masks and respirators.
- Masks and respirators should cover the nose and mouth and not be touched due to their infective potential. Meticulous hand washing should take place before and after mask handling [5].
- Prolonged use of masks and respirators can impact the body's physiology, leading to side effects [27,36].
- Children are particularly vulnerable to the side effects of prolonged mask-wearing. For children under 12, and those under 5 in particular, poor mask behavior is expected [49].
- Disposable masks present lower protection after decontamination and reuse. They should be worn once and recycled to decrease the environmental plastic burden [64].
Conclusion
Face-masks have become a symbol of the pandemic. How well they can reduce community transmission of COVID-19 depends on factors such as type of mask, fitting, mask behavior, and hygiene. Currently, the decision to wear a mask or not is personal. It should take into account the presence of comorbidities, physical and psychological well-being, nature, and duration of social interactions. In general, surgical and cloth masks can protect the wearer for minutes. However, used cloth masks can become a health hazard, increasing the risk of infection. While respirators can offer hours of protection, extended use of masks and respirators can raise health concerns, particularly in children. By weighing the risks against the benefits of facemask wearing, each individual should be able to make a conscious, informed decision.
References
1. Murgolo N, Therien AG, Howell B, Klein D, Koeplinger K, Lieberman LA, et al. (2021) SARS-CoV-2 tropism, entry, replication, and propagation: Considerations for drug discovery and development. PLoS Pathog. 22:753-75.
2. Pearce N, Vandenbroucke JP. (2021) Arguments about face masks and Covid-19 reflect broader methodologic debates within medical science. Eur J Epidemiol. 36(2):143-7.
3. Van Dyke ME, Rogers TM, Pevzner E, Satterwhite CL, Shah HB, et al. (2020) Trends in county-level COVID-19 incidence in counties with and without a mask mandate. MMWR Morb Mortal Wkly. 69(47):1777.
4. Peeples L. (2020) What the data say about wearing face masks. Nature. 586 (7826):186-9.
5. Park AM, Khadka S, Sato F, Omura S, Fujita M, et al. (2022) Bacterial and fungal isolation from face masks under the COVID-19 pandemic. Sci Rep. 12(1):11361.
6. Walensky RP. (2022) CDC streamlines COVID-19 guidance to help the public better protect themselves and understand their risk: EPR.
7. Bhattacharjee S, Bahl P, Chughtai AA, MacIntyre CR. (2020) Last-resort strategies during mask shortages: optimal design features of cloth masks and decontamination of disposable masks during the COVID-19 pandemic. BMJ Open Respir Res. 7(1):e000698.
8. Levine M. (2022) A More Fitting Approach to Mask Policy. Am J Med. 135(11):1280-1.
9. Bar-On YM, Flamholz A, Phillips R, Milo R.(2020) Science,“SARS-CoV-2 (COVID-19) by the numbers,” eLife. 9:e57309.
10. Howard J. Particle sizes for mask filtration. (2020).
11. Lee KW, Liu BY. (1980) On the minimum efficiency and the most penetrating particle size for fibrous filters. J Air Pollut Control Assoc. 30(4):377-81.
12. Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, et al. (2020) Face masks against COVID-19: an evidence review. Proc Natl Acad Sci USA. 118(4):e2014564118.
13. Liao M, Liu H, Wang X, Hu X, Huang Y, et al. (2021) A technical review of face mask wearing in preventing respiratory COVID-19 transmission. Curr Opin. 52:101417.
14. Chua MH, Cheng W, Goh SS, Kong J, Li B, et al. (2020) Face masks in the new COVID-19 normal: materials, testing, and perspectives. Research.
15. Balazy A, Toivola M, Adhikari A, Sivasubramani SK, ReponenT, et al. (2006) Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks?. Am J Infect. Control. 34(2):51-7.
16. Sickbert-Bennett EE, Samet JM, Clapp PW, Chen H, Berntsen J, et al. (2020) Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. JAMA Intern Med. 180(12):1607-12.
17. Rengasamy S, Eimer B, Shaffer RE. (2010) Simple respiratory protection-evaluation of the filtration performance of cloth masks and common fabric materials against 20–1000 nm size particles. Ann Occup Hyg. 54(7):789-98.
18. Neupane BB, Mainali S, Sharma A, Giri B. (2019) Optical microscopic study of surface morphology and filtering efficiency of face masks. Peer J. 7:e7142.
19. Clapp PW, Sickbert-Bennett EE, Samet JM, Berntsen J, Zeman KL, et al. (2021) Evaluation of cloth masks and modified procedure masks as personal protective equipment for the public during the COVID-19 pandemic. JAMA Intern Med. 181(4):463-9.
20. Brainard J, Jones N, Lake I, Hooper L, Hunter PR. (2020) Facemasks and similar barriers to prevent respiratory illness such as COVID-19: A rapid systematic review. Med Rxiv. 6:2020-04.
21. Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. (2013) Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS pathogens. 9(3):e1003205.
22. Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, et al. (2020) Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS nano. 14(5):6339-47.
23. Jung H, Kim JK, Lee S, Lee J, Kim J, et al. (2014). Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual Res. 14(3):991-1002.
24. Collins AP, Service BC, Gupta S, Mubarak N, Zeini IM, et al. (2021) N95 respirator and surgical mask effectiveness against respiratory viral illnesses in the healthcare setting: A systematic review and meta‐analysis. J Am Coll Emerg. Physicians Open:e12582.
25. Centers for Disease Control and Prevention (CDC). (2022) Infect Prev Control Recomm Health Pers Dur Coronavirus Dis Pandemic.
26. Du W, Iacoviello F, Fernandez T, Loureiro R, Brett DJ, et al. (2021) Microstructure analysis and image-based modelling of face masks for COVID-19 virus protection. Commun. Mater. 2(1):1-0.
27. Delanghe L, Cauwenberghs E, Spacova I, De Boeck I, Van Beeck W, et al. (2021) Cotton and surgical face masks in community settings: bacterial contamination and face mask hygiene. Front Med. 8:732047.
28. MacIntyre CR, Seale H, Dung TC, Hien NT, Nga PT, et al.(2015)A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ open. 5(4):e006577.
29. Sharma SK, Mishra M, Mudgal SK. (2020) Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: A systematic review and meta-analysis. J Educ Health Promot. 9.
30. Toomey EC, Conway Y, Burton C, Smith S, Smalle M, et al. (2021) Extended use or reuse of single-use surgical masks and filtering face-piece respirators during the coronavirus disease 2019 (COVID-19) pandemic: A rapid systematic review. Infect Control Hosp Epidemiol. 42(1):75-83.
31. Seresirikachorn K, Phoophiboon V, Chobarporn T, Tiankanon K, Aeumjaturapat S, et al. (2021) Decontamination and reuse of surgical masks and N95 filtering face piece respirators during the COVID-19 pandemic: A systematic review. Infect Control Hosp Epidemiol. 42(1):25-30.
32. Brosseau L, Ulrich A, Escandon K, Osterholm M. (2022) Commentary: What can masks do? Part 1: The science behind COVID-19 protection.
33. https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/respsource3fittest.html
34. Gandhi M, Marr LC. (2021) Uniting infectious disease and physical science principles on the importance of face masks for COVID-19. Med. 2(1):29-32.
35. https://www.cdc.gov/oralhealth/infectioncontrol/guidelines/index.htm
36. Kisielinski K, Giboni P, Prescher A, Klosterhalfen B, Graessel D, et al. (2021) Is a mask that covers the mouth and nose free from undesirable side effects in everyday use and free of potential hazards? IJERPH. 18(8):4344.
37. Mheidly N, Fares MY, Zalzale H, Fares J. (2020) Effect of face masks on interpersonal communication during the COVID-19 pandemic. Front Public Health. 8:582191.
38. İpek S, Yurttutan S, Gullu UU, Dalkıran T, Acıpayam C, et al. (2021) Is N95 face mask linked to dizziness and headache? Int Arch Occup Environ Health. 94(7):1627-36.
39. Lee HP, Wang DY. (2011) Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann Occup Hyg. 55(8):917-21.
40. Harber P, Barnhart S, Boehlecke BA, Beckett WS, Gerrity T, et al. (1996) Respiratory protection guidelines. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors. Am J Respir Crit Care Med. 154(4):1153-65.
41. Matuschek C, Moll F, Fangerau H, Fischer JC, Zanker K, et al. (2020) Face masks: benefits and risks during the COVID-19 crisis. Eur J Med Res. 25(1):1-8.
42. Kyung SY, Kim Y, Hwang H, Park JW, Jeong SH. (2020) Risks of N95 face mask use in subjects with COPD. Respir care. 65(5):658-64.
43. Kao TW, Huang KC, Huang YL, Tsai TJ, Hsieh BS, Wu MS. (2004) The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 103(8):624-8.
44. Thatiparthi A, Liu J, Martin A, Wu JJ. (2021) Adverse Effects of COVID-19 and Face Masks: A Systematic Review. J Clin Aesthet Dermatol. 14(9 Suppl 1):S39.
45. Achanta S, Sasidharan S, Majji D, Uppala D. (2021) “Mask Mouth” During COVID-19 Pandemic-A Myth or A Truth. J Int Dent Medical Res. 1(2):56-63.
46. Liu C, Li G, He Y, Zhang Z, Ding Y. (2020) Effects of wearing masks on human health and comfort during the COVID-19 pandemic. IOP Conf Ser Earth Environ Sci. 531(1):012034.
47. Kanzow P, Dylla V, Mahler AM, Hrasky V, RodigTet, al. (2021) COVID-19 Pandemic: Effect of Different Face Masks on Self-Perceived Dry Mouth and Halitosis. Int J Environ Res Public Health. 18(17):9180.
48. Faria SF, Costa FO, Pereira AG, Cota LO. (2022) Self‐perceived and self‐reported breathe odour and the wearing of face masks during the COVID‐19 pandemic. Oral Dis. 28:2406-16.
49. Spitzer M. (2020) Masked education? The benefits and burdens of wearing face masks in schools during the current Corona pandemic. Trends neurosci educ. 20:100138.
50. Lindsley WG, Blachere FM, Beezhold DH, Law BF, Derk RC, et al. (2021) A comparison of performance metrics for cloth masks as source control devices for simulated cough and exhalation aerosols. Aerosol Sci Technol. 55(10):1125-42.
51. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
52. Courtney JM, Bax A. (2021) Hydrating the respiratory tract: An alternative explanation why masks lower severity of COVID-19. Biophys J. 120(6):994-1000.
53. https://www.who.int/news-room/questions-and-answers/item/q-a-children-and-masks-related-to-covid-19
54. https://www.ecdc.europa.eu/en/covid-19/questions-answers/questions-answers-school-transmission.
55. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html
56. Eberhart M, Orthaber S, Kerbl R. (2021) The impact of face masks on children-A mini review. Acta Paediatrica. 1778-83.
57. Smart NR, Horwell CJ, Smart TS, Galea KS. (2020) Assessment of the wearability of facemasks against air pollution in primary school-aged children in London. Int J Environ Res Public Health. 17(11):3935.
58. Farrer Mackie J, Gray HL, Marshall J, Himmelgreen D, Alkon A, et al. (2022) “I Wear a Mask I Wear It All the Time. The Kids Don’t Wear Masks”: Early Childhood Education Mask-Wearing During COVID-19 in Florida. Health Promotion Practice.15248399221093972.
59. Braga PP, Souza MS, Oliveira PP, Romano MC, Rocha GM, et al. (2022) Children wearing face masks to prevent communicable diseases: scoping review. Revista Paulista de Pediatria. 41.
60. Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, et al. (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA pediatr. 174(9):882-9.
61. Bunyavanich S, Do A, Vicencio A. (2020) Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. Jama. 323(23):2427-9.
62. World Health Organization, WHO. (2020) Advice on the use of masks for children in the community in the context of COVID-19. Geneva: World Health Organization.
63. https://news.mit.edu/2021/covid-masks-environment-0720
64. Selvaranjan K, Navaratnam S, Rajeev P, Ravintherakumaran N. (2021) Environmental challenges induced by extensive use of face masks during COVID-19: A review and potential solutions. Environ Prob. 3:100039.