Early Diagnosis and Selected Evidence Based Protocolized Care on the Prevention and Treatment of Exposure Keratopathy in Critically Ill Patients
Nahla Shaaaban Khalil*
*Professor of critical care and emergency nursing
*Corresponding author: Khalil NS, Professor of critical care and emergency nursing
Citation: Khalil SN. (2024) Early Diagnosis and Selected Evidence Based Protocol zed Care On the Prevention and Treatment of Exposure Keratopathy in Critically Ill Patients. J Clin Pract Med Case Rep. 1(1):1-4.
Received: November 3, 2023 | Published: January 10, 2024
Copyright© 2024 by Khalil NS. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.52793/JCPMCR.2024.1(1)-01
Abstract
Exposure keratopathy (EK) is a frequent encountered complication seen mostly in sedated and mechanically ventilated patients. It is manifested by eye pain and irritation, but can progress rapidly to loss of vision in severe cases. Clinical management of EK can be challenging for both critical care nurses and patients due to the nature of treatment with eye drops and ointments as well as the burden and expense of associated procedural interventions. The most common risk factors include lagophthalmos, chemosis, Bell’s palsy, and congenital deformities. Furthermore, critically ill patients are less prone to be diagnosed due to the focus of the medical staff on life-threatening medical issues over prevention of eye problems. However, the possibility of complications related to EK necessitates that prophylaxis remains a critical and principal component of the care provided to these patients. The most critical preventive measure is education of critical care nurses the latest Evidence Based Protocolized Care on the Prevention and Treatment of Exposure Keratopathy in Critically Ill Patients.
Introduction
Background
Exposure keratopathyis the dryness of the cornea with successive epithelial breakdown. Inadequate closure of eyelid causing evaporation of tears and deficiency of tear film resulting in exposure keratopathy. Mild cases are managed easily, but in severe cases serious complications may happen. Corneal dryness is more prone to be not diagnosed in critically ill patients when other problems are being concentrate on medical issues [1-3]. Exposure keratopathy was identified in 57% of the patients who were being sedated or connected with mechanical ventilation. Moreover, it was noted that 70% of the patients with lagophthalmos had exposure keratopathy. (McHugh et al). Lagophthalmos is the failure to close the eyelids entirely that may be caused by mechanical ventilation, decreased consciousness, administration of paralytics, and prolonged hospitalization are the principal risk factors of EK in patients managed in intensive care units [4-7].
Assessment and Early Diagnosis
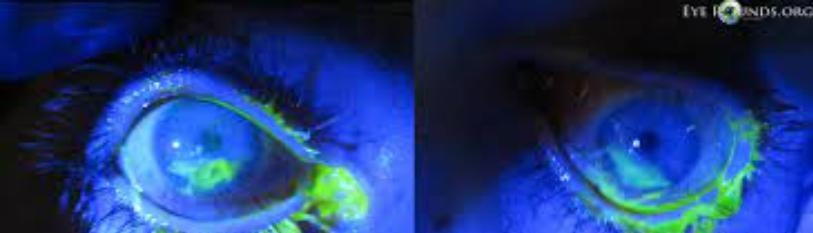
As a result, it has been detected that exposure keratopathy occurred in 13.2% of the patients after they were hospitalized [8]. These ratios propose that eye disorders in ICU patients have to be taken into consideration. No standard or unified eye care protocol is undertaken by ICU staff with respect to the eyes in general unless the clinical findings and eye complications become clearly visible. This result in eye problems during the recovery phase of disease [9-13, 7].Assessment of the vision and ocular function is usually carried out by an ophthalmologist. However, it is difficult to observe or detect the ocular surface of all ICU patients routinely.[14]. Moreover, it is suggested that the cornea could be investigated and assessed for epithelial damage during nursing practices of eye care by the critical care nurse or physician through a fluorescein staining test [15].This test aims to detect the presence of EK by instilling 2% of a small amount of fluorescein drop into each conjunctival sac. The appearance of staining on the cornea provides an indication of the severity of the epithelial damage. Corneal staining is managed in terms of characteristic and grade. The characteristic staining can be punctuate (marked by spots, dots, and points and considered to be clinically less important) or geographical (a more intense defect and considered to be clinically significant). In terms of grade, one-quarter, one-third, or one-half of the corneas can be stained. The greater the degree of corneal staining, the more severe the EK [16-17].Critical care nurses who are in direct contact for longer time with these patients, could detect early and diagnose the problem during the provision of care.
Selected RCT Evaluated Interventions
This frequent assessment would be regularly carried out to prevent undetected eye problems, and complications that are likely to occur in the future. In a study done by [18] who studied the impact of polyethylene cover in patients developed keratopathy utilizing RCT study. They found in the earlier phase of their study, after training, ICU nurses can practice the fluorescein test and detect corneal damage in the early stage. This RCT evaluated interventions to reduce exposure keratopathy in ICU patients and found eye drops plus PC to be more effective and safer than eye drops alone in the treatment. The implementation of effective eye care measures and reducing eye complications are critical roles of ICU nurses. The use of PC together with Carbomer drops (CD) in the treatment of EK could help ICU nurses prevent and treat eye problems. Nurses play a crucial role in applying the best evidence-based practices to improve patients' eye health. We suggest that larger multi-centre studies be conducted comparing PC with other methods for the healing of EK in larger populations. Nurses should be educated on the utilization of PCs in the prevention and management of exposure keratopathy.
References
-
Werli-Alvarenga A, Ercole FF, Botoni FA, Oliveira JADMM. (2011) Corneal injuries: Incidence and risk factors in the intensive care unit. Rev Lat Am Enfermagem. 19(5):1088–95.
-
Kuruvilla S, Peter J, David S, Prem kumar PS, Ramakrishna K, et al. (2015) Incidence andrisk factor evaluation of exposure keratopathy in critically ill patients: A cohort study. J Crit Care. 30(2):400–404.
-
Oliveira RS, Fernandes APNL, Botarelli FR, Araujo JNM, Bareto VP, et al. (2016) Risk factors for injury in the cornea in critical care patients in intensive care: An integrative review. Journal of Research Funda.
-
Grixti A, Sadri M, Edgar J, Datta AV. (2012) Common ocular surface disorders in patients in intensive care units. Ocul Surf. 10(1):26-42.
-
Alavi NM, Sharifitabar Z, Shaeri M, Hajbaghery MA. (2013) An audit of eye dryness and corneal abrasion in ICU patients in Iran. Nurs Crit Care. 19(2):73-77.
-
Wekken RJ, Torn E, Ros FE, LEM H. (2013) A red eye on the intensive care unit. Exposure keratopathy with corneal abrasion secondary to lagophthalmos due to chemosis. Neth J Med. 71(4):204-7
-
Oliveira RS, Fernandes APNL, Botarelli FR, Araújo JNM, Barreto VP, et al. (2016) Risk factors for injury in the cornea in critical patients in intensive care: an integrative review. J Res Fundam Care Online. 8(1): 4423-34.
-
https://corescholar.libraries.wright.edu/nursing_dnp/
-
Alansari MA, Hijazi MH, Maghrabi KA. (2015) Making a difference in eye care of the critically ill patients. J Intensive Care Med. 30(6):311–17.
-
Kousha O, Kousha Z, Paddle J. (2015) The risk factors for developing exposure keratopathy in ICU patients. Intensive Care Med Exp. 3(Suppl 1):A731.
-
Kuruvilla S, Peter J, David S, Premkumar PS, Ramakrishna K, et al. (2015) Incidence and risk factor evaluation of exposure keratopathy in critically ill patients: A cohort study. J Critical Care. 30(2):400–404.
-
de França CF, Fernandes AP, Carvalho DP, de Mesquita Xavier SS, et al. (2016) Evidence of interventions for the risk of dry eye in critically ill patients: An integrative review. Appl Nurs Res. 29:e14–e17.
-
Güler EK, Es¸er I, Fashafsheh IHD. (2016) Intensive care nurses’ views and practices for eye care: An international comparison. Clin Nurs Res. 26(4):504-24.
-
McHugh J, Alexander P, Kalhoro A, Iodines A. (2008) Screening for ocular surface disease in the intensive care unit. Eye (Lond). 22(12):1465–68.
-
Demirel S, Cumurcu T, Fırat P, Aydogan MS. Doganay S. (2014) Effective management of exposure keratopathy developed in intensive care units: The impact of an evidence based eye care education programme. Intensive Crit Care Nurs. 30(1):38–44.
-
Güler EK, EserI Egrilmez S. (2018) Nurses can play an active role in the early diagnosis of exposure keratopathy in intensive care patients. Jpn J Nurs Sci. 15(1):31-38.
-
Kocaçal E, EserI Egrilmez S. (2021) Effect of polyethylene cover on the treatment of exposure keratopathy in ICU. Nurs Crit Care. 26(4):282- 87.

