COVID-19-Associated Acute Necrotizing Pancreatitis: A Case Report
Ahmed Yagoub Ahmed Mohammed*
General Physician, MBBS, USMLE
*Corresponding author: Ahmed Yagoub Ahmed Mohammed, General Physician, MBBS, USMLE.
Citation: Mohammed AYA. COVID-19-Associated Acute Necrotizing Pancreatitis: A Case Report. Adv Clin Med Res. 6(1):1-4.
Received: January 07, 2025 | Published: April 18, 2025
Copyright© 2025 genesis pub by Mohammed AYA. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/ACMR.2025.6(1)-94
Abstract
COVID-19, caused by SARS-CoV-2, was declared a pandemic by the WHO on March 11, 2020. While primarily a respiratory illness, gastrointestinal (GI) symptoms such as nausea, vomiting, and diarrhea are increasingly recognized. Emerging evidence suggests SARS-CoV-2 may cause pancreatic injury or acute pancreatitis (AP), likely due to its interaction with the ACE2 receptor expressed in pancreatic tissue. This case report describes a 53-year-old male with acute necrotizing pancreatitis secondary to COVID-19 infection, with no other identifiable risk factors, highlighting a potential direct association between SARS-CoV-2 and severe pancreatic damage.
Keywords
SARS-CoV-2; COVID-19 infection; Pancreatic damage; Acute necrotizing.
Introduction
COVID-19, caused by SARS-CoV-2, primarily presents with respiratory symptoms but is increasingly associated with GI manifestations [1]. Viral infections, including cytomegalovirus and Epstein-Barr virus, are known causes of AP. SARS-CoV-2 binds to the ACE2 receptor, which is highly expressed in the pancreas, suggesting a potential mechanism for pancreatic injury [2]. This report presents a case of acute necrotizing pancreatitis in a patient with recent COVID-19 infection, emphasizing the possible link between SARS-CoV-2 and pancreatic damage.
Case presentation
A 53-year-old male with a history of End-Stage Renal Disease (ESRD) on dialysis, atrial fibrillation, and a prior cerebrovascular accident was admitted with recurrent vomiting, hypotension, and abdominal distension. Laboratory and imaging findings confirmed acute necrotizing pancreatitis. The patient had no other risk factors for AP, such as gallstones, alcohol abuse, or hypertriglyceridemia, suggesting COVID-19 as the likely cause.
Diagnostic criteria for acute pancreatitis
The diagnosis of acute pancreatitis was based on the following criteria:
Laboratory results
Key laboratory findings are summarized below:
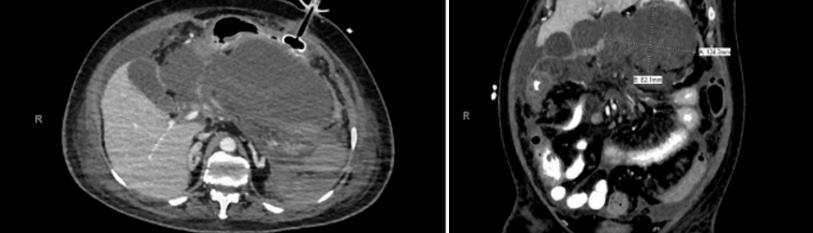
Imaging findings
Figure 1: CT Abdomen (10/5/23), Severe necrotizing pancreatitis with peri-pancreatic fluid collection.
Figure 2: X-ray Abdomen, Sentinel loop (colon cut-off sign).
ICU Management
The patient was admitted to the ICU and managed with:
- Hemodynamic stabilization: Intravenous fluids and inotropic support.
- Broad-spectrum antibiotics: Meropenem, vancomycin, amikacin, metronidazole.
- Renal support: Continuous Renal Replacement Therapy (CRRT).
- Nutritional support: Total Parenteral Nutrition (TPN) due to intolerance to enteral feeding.
- Monitoring: Serial intra-abdominal pressure (IAP) measurements to rule out abdominal compartment syndrome.
Discussion
Acute pancreatitis is an inflammatory condition of the pancreas with high morbidity [3]. In this case, the patient presented with no traditional risk factors for AP, suggesting COVID-19 as the likely cause. SARS-CoV-2 binds to ACE2 receptors in pancreatic tissue, potentially leading to direct viral injury or systemic inflammation [4]. Elevated D-dimer levels and cytokine storms may also contribute to pancreatic damage [5].
The Ranson score, used to assess AP severity, indicated a poor prognosis in this case. Key findings included elevated WBC, LDH, and creatinine, along with hypocalcemia and fluid sequestration [6].
Conclusion
This case highlights the potential for SARS-CoV-2 to cause severe pancreatic injury, even in the absence of traditional risk factors. Further research is needed to understand the mechanisms underlying COVID-19-associated pancreatitis and to develop targeted management strategies.

