Choledocholithiasis Presents a Significant Challenge and Carries a Considerable Risk of Various Complications; a Comparative Study Determining Efficacy of ERCP and MRCP in Managing CBD Obstruction
Nayab Mustansar1*, Tariq Saeed Siddique2 and Asma Asghar3
1Resident Radiology, Department of Radiology, Combined Military Hospital Peshawar
2Consultant Radiologist, Department of Radiology, Combined Military Hospital Peshawar
3Consultant Gastroenterologist, Combined Military Hospital Peshawar
*Corresponding author: Nayab Mustansar, Resident Radiology, Department of Radiology, Combined Military Hospital Peshawar
Citation: Mustansar N, Siddique TS and Asghar A. Choledocholithiasis Presents a Significant Challenge and Carries a Considerable Risk of Various Complications; a Comparative Study Determining Efficacy of ERCP and MRCP in Managing CBD Obstruction. J Clin Pract Med Case Rep. 1(1):1-11.
Received: May 1, 2024 | Published: May 23, 2024.
Copyright© 2024 genesis pub by Mustansar N. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Objective: This study aims to compare the diagnostic efficacy of MRCP and ERCP in the management of choledocholithiasis through a comprehensive analysis of 20 patients.
Study design: It is a cross sectional prospective study carried out in the Radiology department of CMH Peshawar for a span of three months from January 2024 – March 2024.
Setting: Radiology department of CMH Peshawar. STUDY DURATION: 1st January 2024- 1st March 2024.
Methodology: A group of 20 patients were selected using a non-probability purposive sampling method for this study. The criteria for inclusion were patients aged between 15- and 80-years exhibiting signs and symptoms of obstructive jaundice and abdominal ultrasonography showing CBD stones.
Exclusion criteria comprised patients with claustrophobia, a documented allergic response to contrast agent, impaired renal function, or disseminated metastatic disease. Each patient underwent a comprehensive assessment including medical history, physical examination, and laboratory tests (including BCP, LFT’s, and Coagulation profile). Subsequently, all patients having CBD stones on abdominal ultrasound underwent MRCP, which was conducted utilizing a 1.5 Tesla MRI machine. The interpretation of MRCP findings was carried out by a single consultant radiologist who assessed the presence or absence of CBD stones. Finally, ERCP procedures were performed on the same patients by a skilled gastroenterologist, during which lesion visualization, biopsy, and appropriate interventions were executed. Comparative analysis of MRCP and ERCP was carried out.
Results: Sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of both MRCP and ERCP were calculated and compared. Procedural complications were calculated and compared as well. CONCLUSION: This study concluded that MRCP, being non-invasive, is particularly valuable in the pre-surgical assessment of patients with obstructive jaundice because of its higher sensitivity. Although ERCP is an invasive procedure, still has got better specificity, Negative predictive value, positive predictive value and accuracy as compared to MRCP.
Keywords
Common bile duct (CBD), Jaundice, Magnetic Resonance Cholangiopancreatography, Obstructive Jaundice, Endoscopic retrograde cholangiopancreatography.
Introduction
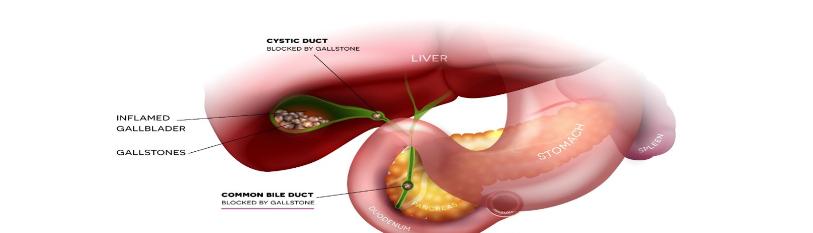
Choledocholithiasis, the presence of gallstones within the bile duct, poses a significant clinical challenge due to its potential complications including biliary obstruction, pancreatitis, and cholangitis. Accurate diagnosis and management are crucial to prevent complications and improve patient outcomes [1]. MRCP and ERCP are widely utilized diagnostic tools in the evaluation of choledocholithiasis, each with its advantages and limitations. Biliary obstruction can stem from various causes such as choledocholithiasis, tumours and post-gall bladder surgery trauma, with choledocholithiasis being the primary culprit [2]. In England and Wales, the prevalence of gallstones was 182 per 10,000 person-years at risk, with an incidence rate of 8 per 10,000 person-years at risk for 1991–1992. Patients exhibiting symptoms like abnormal liver function, jaundice, pale stools, dark urine, itching, upper right quadrant abdominal pain, fever, nausea, and vomiting are indicative of suspected biliary obstruction [3]. Endoscopic ultrasonography (EUS) serves as the initial imaging investigation for patients with jaundice or right upper-quadrant pain. However, EUS's efficacy is highly dependent on the operator and patient [4].
Endoscopic retrograde cholangiopancreatography (ERCP) stands as the current 'gold standard' for diagnosing biliary obstruction but isn't flawless, prompting the exploration of alternative diagnostic approaches [5]. Magnetic resonance cholangiopancreatography (MRCP) serves as a non-invasive alternative for imaging the biliary tree and investigating biliary obstruction. MRCP, developed in 1991, continues to evolve, offering a feature-rich diagnostic tool without the therapeutic capabilities of ERCP, and without its associated morbidity and mortality [6]. MRCP usage may circumvent unnecessary invasive procedures such as ERCP [7].
Indications for MRCP usage include unsuccessful or contraindicated ERCP, patient preference for non-invasive imaging, low-risk patients for pancreatic or biliary disease, unlikely therapeutic ERCP need, and suspected neoplastic causes for obstruction. MRCP requires no patient preparation and typically doesn't necessitate sedation [8-10]. It serves as a valuable option for challenging ERCP cases and failed procedures. ERCP and MRCP, with differing contraindications, complement each other effectively [11,12].
A systematic review comparing MRCP to ERCP was conducted to ascertain their sensitivity and specificity. This paper presents the findings of MRCP compared to diagnostic ERCP in investigating biliary obstruction, focusing on accuracy statistics, study quality, population characteristics, and suspected conditions. The discussion primarily centers on the diagnosis of choledocholithiasis, the most prevalent cause of biliary obstruction [13,14].
Methodology
The study, conducted by the Radiology department at CMH Peshawar, spanned from January 1st, 2024, to March 1st, 2024, following approval from the institutional ethical review committee. The sample size was determined using a sensitivity-specificity calculator. A total of 20 patients who met the inclusion criteria presented to the Radiology department of CMH Peshawar were selected. Informed consent was obtained from each patient.
All with CBD stones on abdominal ultrasound underwent MRCP conducted on a 1.5-T system. The MRCP findings were interpreted by a consultant radiologist with at least 3 years of experience, searching for CBD stones according to the pre-defined criteria. Finally, ERCP procedures were carried out on the same patients by an expert gastroenterologist, including lesion visualization, biopsy, and necessary interventions. Comparative analysis was done for both MRCP and ERCP.
All relevant data (such as age, gender, laboratory investigations including LFT’s and Coagulation profile, duration of symptoms, presence of CBD stones on transabdominal USG, MRCP findings, and ERCP findings) as per the operational definition, were recorded on a specially designed proforma.
Inclusion criteria encompassed both genders aged between 15-85 years exhibiting signs and symptoms of obstructive jaundice and USG findings of CBD stones. Exclusion criteria comprised patients with known allergic reactions to contrast agents, impaired renal functions (GFR <30 and creatinine >1.3 mg/dl), claustrophobia, or disseminated metastatic disease.
Data collected was analysed using SPSS 25.0 software and excel sheet. Diagnostic parameters including accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. Additionally, procedural complications associated with each modality were documented.
Our data included 11 male patients and 9 female patients as shown below in (figure1).
Figure 1: Male to female ratio (Collected Data).
Out of there 20 patients 10 were having normal LFT’s whereas 10 were having deranged LFT’s as shown in (Figure 2).
Figure 2: Liver Function Tests (Collected Data).
Results
The diagnostic accuracy of MRCP and ERCP was compared, revealing differences in sensitivity, specificity, PPV, and NPV. Statistical analysis was performed to assess the significance of these differences. Additionally, procedural complications such as pancreatitis, bleeding, and perforation were analysed for both modalities.
The sensitivity, specificity, NPV and PPV along with accuracy is described below for both ERCP and MRCP. The parameters for MRCP are shown in (Table 1).
|
Statistic |
Value |
95% CI |
|
Sensitivity |
90.00% |
80.49% to 100.00% |
|
Specificity |
75.00% |
11.81% to 88.19% |
|
Positive Likelihood Ratio |
2 |
0.90 to 4.45 |
|
Negative Likelihood Ratio |
0 |
0 |
|
Disease prevalence (*) |
73.91% |
51.59% to 89.77% |
|
Positive Predictive Value (*) |
85.00% |
71.80% to 92.65% |
|
Negative Predictive Value (*) |
100.00% |
29.24% to 100.00% |
|
Accuracy (*) |
86.96% |
66.41% to 97.22% |
Table 1: Statistical Analysis of sensitivity and specificity of MRCP.
The sensitivity of MRCP in diagnosing CBD stones is quite good as compared to its specificity and PPV. However, the accuracy is 89.6 % which is good enough for refereeing a patient for further invasive procedure or intervention. Similarly, that of ERCP shows the diagnostic parameters as under shown in (Table 2).
|
Statistic |
Value |
95% CI |
|
Sensitivity |
95.00% |
76.84% to 100.00% |
|
Specificity |
80.67% |
22.28% to 95.67% |
|
Positive Likelihood Ratio |
3 |
0.97 to 9.30 |
|
Negative Likelihood Ratio |
0 |
0 |
|
Disease prevalence (*) |
70.00% |
45.72% to 88.11% |
|
Positive Predictive Value (*) |
87.50% |
69.30% to 95.60% |
|
Negative Predictive Value (*) |
100.00% |
39.76% to 100.00% |
|
Accuracy (*) |
90.00% |
68.30% to 98.77% |
Table 2: Statistical Analysis of sensitivity and specificity of ERCP.
By comparing the diagnostic parameters of both ERCP and MRCP as shown in Table :3. It is clearly seen that the sensitivity of MRCP for CBD stones is more than that of ERCP. However, specificity, PPV and accuracy of ERCP is more than that of MRCP.
|
Diagnostic Parameter |
MRCP (%) |
ERCP (%) |
|
Sensitivity |
80 |
76 |
|
Specificity |
88 |
95 |
|
PPV |
85 |
87 |
|
NPV |
100 |
100 |
|
Accuracy |
86 |
90 |
Table 3: Comparison of Diagnostic Parameters between MRCP and ERCP.
Comparative analysis of both MRCP and ERCP is shown as under in (Figure 3).
Figure 3: Comparative Analysis of Sensitivity between MRCP and ERCP.
It is obvious from the Table:3 and Figure:3 that the diagnostic sensitivity of MRCP ais more than that of ERCP however they both have almost equal Negative predictive value. However, the diagnostic Specificity, PPV and accuracy of ERCP is more than that of MRCP.
Following the procedures of MRCP and ERCP, few complications were encountered like bleeding, perforation and pancreatitis their prevalence in each is shown as under in (Table 4).
|
Complication |
MRCP (%) |
ERCP (%) |
|
Pancreatitis |
1 |
2 |
|
Bleeding |
1 |
3 |
|
Perforation |
0 |
1 |
Table 4: Procedural Complications Associated with MRCP and ERCP.
It can be seen clearly that the complications are more with the invasive procedures as compared to that of invasive ERCP.
It can be represented as shown in (Figure 4).
Figure 4: Comparative Analysis of Procedural complications between MRCP and ERCP.
The above diagram clearly shows the least complications with the MRCP as compared to invasive ERCP.
The assessment of CBD via MRCP is shown in (Figure 5) as below.
Figure 5: MRCP assessment results.
Similarly, ERCP assessment of patients is shown in (Figure 6) as below.
Figure 6: ERCP assessment results.
Discussion
Our study highlights the strengths and limitations of MRCP and ERCP in choledocholithiasis diagnosis. Factors influencing diagnostic accuracy and procedural complications were also discussed and addressed. Optimal utilization of each modality in clinical practice is elucidated, considering patient characteristics and institutional expertise [15,16].
According to MRCP showed sensitivity of 95% and Specificity of 85% in diagnosing CBD dilatation irrespective of stone and sludge [31]. MRCP showed PPV 91% and sensitivity of about 89% in detecting the same [32]. Research by (2020) reported excellent diagnostic accuracy of ERCP with high sensitivity 89%) and specificity (96%), but cautioned against its routine use due to associated risks [33]. A study by demonstrated high sensitivity (88%) and specificity (78%) of MRCP in detecting CBD stones, making it a valuable tool for initial screening and diagnosis [34]. Another study by Wang et al. (2013) concluded that MRCP can serve as a reliable initial screening tool, with ERCP reserved for cases where therapeutic intervention is required or when MRCP findings are inconclusive.
Comparing Endoscopic Retrograde Cholangiopancreatography (ERCP) and Magnetic Resonance Cholangiopancreatography (MRCP) involves evaluating various aspects, including diagnostic accuracy, invasiveness, complications, cost-effectiveness, and availability [17,18]. Here, I will discuss these aspects to provide a comprehensive comparison between the two modalities [19]. ERCP is considered the gold standard for diagnosing common bile duct (CBD) stones due to its direct visualization and therapeutic capabilities. MRCP, a non-invasive imaging technique, provides high-quality images of the biliary system, making it an excellent diagnostic tool with sensitivity and specificity comparable to ERCP, especially for detecting larger stones [20,21]. ERCP is an invasive procedure involving the insertion of an endoscope through the mouth, esophagus, stomach, and into the duodenum to access the biliary and pancreatic ducts [23]. MRCP is entirely non-invasive and does not require the insertion of instruments into the body [24]. It utilizes magnetic resonance imaging (MRI) to obtain detailed images of the biliary system [25]. ERCP carries risks of complications, including pancreatitis, bleeding, perforation, infection, and reaction to contrast agents [26]. These complications can range from mild to severe and may require additional interventions or hospitalization [27]. MRCP is generally considered safer as it does not involve any invasive procedures or the use of contrast agents, thereby significantly reducing the risk of complications [28]. ERCP is typically more expensive than MRCP due to the need for specialized equipment, sedation/anaesthesia, and the potential for complications that may require additional medical care. MRCP, while initially costly due to the equipment and technician expertise required, may prove to be more cost-effective in the long run due to its non-invasive nature and lower risk of complications [29,30]. ERCP requires specialized endoscopic equipment and trained personnel, limiting its availability to tertiary care centers or hospitals with gastroenterology departments. MRCP is more widely available since it relies on standard MRI machines found in most hospitals and imaging centres [31]. It can be performed by radiology departments, enhancing accessibility for patients in various healthcare settings. The choice between ERCP and MRCP depends on various factors, including the patient's clinical condition, the urgency of diagnosis, the presence of contraindications to invasive procedures, and local expertise and resources. In cases where therapeutic intervention is needed (e.g., stone extraction, stent placement), ERCP remains the preferred modality despite its invasiveness and associated risks. MRCP is often utilized as an initial non-invasive screening tool, especially in stable patients without urgent therapeutic needs or those at higher risk of complications from invasive procedures.
Conflict of interest
None.
Conclusion
Study concluded that both MRCP and ERCP play crucial roles in choledocholithiasis diagnosis, with distinct advantages. The choice between modalities depends on various factors. Our study shows that the MRCP has good diagnostic sensitivity for CBD stones however the Diagnostic specificity, PPV and accuracy of ERCP is still higher than MRCP. Although the complications of invasive ERCP are more as compared to MRCP. This study provides valuable insights into diagnostic efficacy and procedural outcomes, guiding clinical decision-making in choledocholithiasis management.
References
-
Roche SP, Kobos R. (2004) Jaundice in the adult patient. Am Fam Physician. 69(2):299-304.
-
Beers MH, Berkow R. (1999) Hepatic and biliary disorders. In: Beers MH, Berkow R, editors. The Merck manual of diagnosis and therapy. 17th ed. Whitehouse Station (NJ): Merck & Co; 1999.
-
Ahmad I, Jan AU, Ahmad R. (2001) Obstructive jaundice. J Postgrad Med Inst. 15:194-98.
-
Nadkarni KM, Jahagirdar RR, Kagzi RS, Pinto AC, Bhalerao RA. (1981) Surgical obstructive jaundice. J Postgrad Med 27(1):33-39.
-
Kahnag KU, Roslyn JJ. (2001) Jaundice Maingot’s abdominal operations. Vols. I and II. 10th ed. Singapore: McGraw Hill. 1701-31.
-
Honickman SP, Mueller PR, Witternberg J, Simeone JF, Ferrucci JT, et al. (1983) Ultrasound in obstructive jaundice: prospective evaluation of site and cause. Radiology. 147(2):511-15.
-
Martin DF, Laasch HU. (2001) The biliary tract. In: Grainger RG, Allison D, editors. Grainger and Allison’s diagnostic radiology – a textbook of medical imaging. 4th ed. London: Churchill Livingstone, Harcourt Publishers Limited.
-
Patel JC, McInnes GC, Bagley JS, Needham G, Krukowski ZH. (1993) The role of intravenous cholangiography in preoperative assessment for laparoscopic cholecystectomy. Br J Radiol. 66(792):1125-27.
-
Wallner BK, Schumacher KA, Weidenmaier W, Fariedrich JM. (1991) Dilated biliary tract: evaluation with MR cholangiography with a T2 weighted contrast-enhanced fast sequence. Radiology. 181(3):805-808.
-
Gameraddin M, Abdalgaffar R, Yousef M. (2013) The role of ultrasound in diagnosis of obstructive jaundice causes in Sudanese population. IOSR J Nurs Health Sci. 1:25-28.
-
Sharma MP, Ahuja V. (1999) Aetiological spectrum of Obstructive jaundice and diagnostic ability of ultrasonography: a clinician’s perspective. Trop Gastroenterol. 20(4):167-69.
-
Moghimi M, Marashi SA, Salehian MT, Sheikhvatan M. (2008) Obstructive jaundice in Iran: factors affecting early outcome. Hepatobiliary Pancreat Dis Int. 7(5):515-19.
-
Huang JQ, Bao XJ, Lu XH. The common causes and differential diagnosis of malignant jaundice. Zhonghua Nei Ke Za Zhi. 32(6):400-404.
-
Saluja SS, Sharma R, Pal S, Sahni P, Chattopadhyay TK. (2007) Differentiation between benign and malignant hilar obstructions using laboratory and radiological investigations: a prospective study. HPB. 9(5):373-82.
-
Siddique K, Ali Q, Mirza S, Jamil A, Ehsan A, et al. (2008) Evaluation of the aetiological spectrum of obstructive jaundice. J Ayub Med Coll Abbottabad. 20(4):62-66.
-
Park MS, Yu JS, Kim YH, Kim MJ, Kim JH, et al. (1998) Acute cholecystitis: comparison of MR cholangiography and US. Radiology. 209(3):781-85.
-
Chalya PL, Kanumba ES, Mchembe M. (2011) Etiological spectrum and treatment outcome of obstructive jaundice at a University teaching Hospital in northwestern Tanzania: a diagnostic and therapeutic challenges. BMC Res Notes. 4:147.
-
Verma S, Sahai S, Gupta P, Munshi A, Verma S, et al. (2010) Obstructive jaundice – aetiological spectrum, clinical, biochemical and radiological evaluation at a tertiary care teaching hospital. Internet J Trop Med. 7(2).
-
Verghese JC, Farrell MA, Courtney G, Osborne H, Murray FE, et al. (1999) A prospective comparison of MRCP with ERCP in the evaluation of patients with suspected biliary tract diseases. Clin Radiol. 54(8):513-20.
-
Kim MJ, Han SJ, Yoon CS, Kim JH, Oh JT, et al. (2002) Using MR cholangiopancreatography to reveal anomalous pancreaticobiliary ductal union in infants and children with choledochal cysts. AJR Am J Roentgenol. 179(1):209-14.
-
Laokpessi A, Bouillet P, Sautereau D, Cessot F, Desport JC, et al. (2001) Value of magnetic resonance cholangiography in the preoperative diagnosis of common bile duct stones. Am J Gastroenterol. 96(8):2354-59.
-
Soto JA, Barish MA, Alvarez O, Medina S. (2000) Detection of choledocholithiasis with MR cholangiography: comparison of 3D FSE and single and multisection half Fourier rare sequences. Radiology. 215(3):737-45.
-
Suthar M, Purohit S, Bhargav V, Goyal P. (2015) Role of MRCP in differentiation of benign and malignant causes of biliary obstruction. J Clin Diagn Res. 9(11):TC08-TC12.
-
Bhatt C, Shah PS, Prajapati HJ, Modi J. (2005) Comparison of diagnostic accuracy between USG and MRCP in biliary and pancreatic pathology. Indian J Radiol Imaging. 5(2):177-81.
-
Raguraman P. (2015) MRI combined with MRCP versus helical CT in evaluation of patients with obstructive jaundice. Int J Recent Sci Res. 6(4):3642-50.
-
Al-Obaidi S, Al-Hilli MRA, Fadhel AA. (2007) The role of ultrasound and magnetic resonance imaging in the diagnosis of obstructive jaundice. Imaging Diagn Obstruct Jaundice. 6(1):7-17.
-
Yattoo GN, Amin WG, Shaheen FA, Zargar S, Javid G. (2014) The efficacy of magnetic resonance cholangiopancreatography in assessing the etiology of acute idiopathic pancreatitis. Int J Hepatobiliary Pancreat Dis. 4:32-39.
-
Katabathina VS, Dasyam AK, Dasyam N, Hosseinzadeh K. (2014) Adult bile duct strictures: role of MR imaging and MR cholangiopancreatography in characterization. Radiographics. 34(3):565-86.
-
Angulo P, Pearce DH, Johnson CD, Henry JJ, LaRusso NF, et al. (2000) Magnetic resonance cholangiography in patients with biliary disease: its role in primary sclerosing cholangitis. J Hepatol. 33(4):520-27.
-
Singh A, Mann HS, Thukral CL, Singh NR. (2014) Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. J Clin Diagn Res. 8(3):103-107.
-
Chan YL, Chan AC, Lam WW, Lee DW, Chung SS, et al. (1996) Choledocholithiasis: comparison of MR cholangiography and endoscopic retrograde cholangiography. Radiology. 200(1):85–9.
-
Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H, Hammerstingl R, et al. (1997) Clinical significance of magnetic resonance cholangiopancreatography (MRCP) compared to endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy. 29(03):182–7.
-
Smith ZL, Nickel KB, Olsen MA, Vargo JJ, Kushnir VM. (2020) Type of sedation and the need for unplanned interventions during ERCP: analysis of the clinical outcomes research initiative national endoscopic database (CORI-NED). Frontline Gastroenterol. 11(2):104-10.
-
Jiwani MS, Banode P, Kharche AD, Jiwani AA, Vaidhya SV. (2016) Role of magnetic resonance cholangiopancreatography in cases of obstructive jaundice in correlation with ultrasonography. Int J Recent Surg Med Sci. 2(02):70-84.
-
Bian Y, Wang L, Chen C, Lu JP, Fan JB, et al. (2013) Quantification of pancreatic exocrine function of chronic pancreatitis with secretin-enhanced MRCP. World J Gastroenterology: WJG. 19(41):7177.

